Congestive Heart Failure
Types of medications used to treat CHF Cardiotonic like cardiac glycosides (Digitalis) their mechanism of action, therapeutic and pharmacological effects and potential side effects.
Alok Bains
2/16/202513 min read
Drugs Used in Congestive Heart Failure (CHF): Cardiotonic, Cardiac Glycoside; Digitalis.
Index
Causes of CHF
Types of CHF
Stages of CHF
Symptoms of CHF
Drugs used in CHF
Cardiac glycosides
Pharmacokinetics
Mechanism of action
Pharmacological effects
Digitalis toxicity and treatment
Frank Sterling Mechanism
congestive heart failure (CHF) is a chronic and progressive condition in which the heart muscle is unable to pump blood effectively to meet the organs’ demand for oxygen and nutrients to maintain normal metabolic activity. CHF results in blood returning faster to the heart atria than blood pumped from the heart ventricles, which causes cardiac, pulmonary and systemic congestion. This results in fluid licks from the blood capillaries to a progressive stage of fluid buildup pulmonary, legs, ankles, and feet oedema. Heart failure does not indicate the heart stops working. Here, the heart does not pump enough blood to meet body requirements.
Causes of CHF:
· CVS Related Causes: Myocarditis, pericarditis, heart muscle parasites, heart valve disorder, previous heart attack, faulty impulse conduction in the heart wall, coronary artery disease, artery narrowing, untreated high blood pressure, anaemia and heart attack.
· Pulmonary embolism
· Other causes: Kidney disorders, Type 2 diabetes, thyroid problems,
Types of CHF
Left-sided heart failure: The left ventricle does not pump enough blood to meet the body’s needs. This causes blood accumulation in the pulmonary vein bringing oxygenated blood to the left atria and ventricle. This results in shortness of breath, breathing problems and coughing. It exaggerates during physical activity. It develops due to an increase in the thickness of the ventricle wall and a decrease in the size of the left ventricle. Left-sided heart failure is of the following two types:
Systolic heart failure: The inability of the left ventricle to contract forcefully to pump blood develops systolic heart failure. It is due to weakness in cardiac muscles in the left ventricle wall.
Diastolic heart failure: The inability of the left ventricle to relax completely and to fill blood properly between heartbeats develops diastolic heart failure. It is due to stiffness in cardiac muscles in the left ventricle wall.
Right-sided heart failure: The inability of the right ventricle to pump enough blood to the lungs develops right-sided heart failure. Right-sided heart failure promotes blood accumulation in the vein and fluid leakage from the vein into surrounding tissues especially in the legs.
Biventricular heart failure: The inability of both sides of the heart to pump enough blood is biventricular heart failure. It shows symptoms of both left-sided heart failure and right-sided heart failure.
Stages of CHF
Congestive heart failure has four stages from pre-heart failure to advanced heart failure. Congestive heart failure is classified based on the severity of symptoms:
Stage A CHF or Stage I or Pre heart failure stage: People have no structural and functional heart disorders; no symptoms of heart disorder and no effect on daily life but are at high risk for developing heart failure in the future. People may have breathing problems when lying down due to fluid accumulation. Lifestyle changes and minor medications can manage it.
Stage B CHF or Stage II: People have a structural heart disorder, but no CHF symptoms at any stage. Shortness of breath, palpitation and fatigue during physical activities. Lifestyle changes and minor medications can manage it. It requires more monitoring than stage I.
Stage C CHF or Stage III: People have previous or current heart failure symptoms due to structural heart problems, but managed with medical treatment. Shortness of breath, palpitation and fatigue are more severe than stage II during physical activities. Even simple walking results in respiratory distress. It requires close monitoring by healthcare providers.
Stage D CHF or Stage IV or Advance Stage: Physical activities become impossible. It requires sitting or sleeping upright on the bed to feel comfortable. People have advanced heart disorders and require hospital-based support, a heart transplant, or palliative care. Treatment’s main focus is on the person’s comfort.
Symptoms of CHF:
· Respiratory Symptoms: Rapid breathing (tachypnoea), breathlessness or shortness of breathing (dyspnoea), breathing spasms with a wheezing sound, night attacks of breathlessness (nocturnal dyspnoea), bluish skin (cyanosis), more often hacking and dry coughing while lying down,
· CNS Symptoms: Disorientation and brain fogging, fatigue feeling on slight physical activities, fainting and dizziness, feeling of anxiety and restlessness with suffocation.
· Oedema: Swelling in legs and feet, weight gain. Weight loss due to poor nutrient absorption from GIT.
Drugs Used in Congestive Heart Failure (CHF)
The drugs most commonly used in congestive heart failure are
Cardio tonics: Cardiac glycosides such as digoxin
ACE inhibitors: Benazepril (Lotensin), Captopril (Capoten), Enalapril (Vasotec), Fosinopril (Monopril), Lisinopril (Zestril), Moexipril (Univasc), Perindopril (Aceon), Quinapril (Accupril), Ramipril (Altace).
Angiotensin Receptor Blockers: Valsartan (Diovan), Losartan (Cozaar), Irbesartan (Avapro), Candesartan (Atacand), Telmisartan (Micardis)
Diuretics.
Cardiac Glycosides
Cardiac glycosides are a group of chemically similar organic compounds that increase cardiac muscle contraction and cardiac output without increasing muscle oxygen consumption. Most of the cardiac glycosides are obtained from plant digitalis. Thus, they are also called digitalis glycosides. Plant Digitalis purpurea and Digitalis lanata are sources of cardiac glycosides. Active constituents of Digitalis are digitoxin, digoxin, gitoxin and gitalin. Digoxin and digitoxin are therapeutically active cardiac glycosides. Toad skin and yellow oleander (vetianut) are also sources of cardiac glycosides. Cardiac glycosides act as cardiotonic. Cardiotonics increase the heart muscle contraction efficiency.
Pharmacokinetics of cardiac glycosides (digitalis)
Digoxin is a more polar compound, and its absorption from GIT is more variable and depends upon the source of digoxin, GIT contents, and dissolution of its dosage form. Thus, one dosage form from the same manufacturer should be preferred. Digitalis glycoside concentration in cardiac muscles, skeletal muscles, liver, and kidney remains higher than its concentration in other parts of the body.
Digitoxin is metabolized in the liver to digoxin, which is the active metabolite of digitoxin but less potent than digitoxin. Digitoxin also undergoes enterohepatic circulation and is reabsorbed from the intestine into the liver. This contributes to the cumulative effect of digitalis, which is due to the combined effects of both digitoxin and digoxin. Therefore, the digitoxin dose should be adjusted carefully.
· The onset of action: The onset of action for digitoxin and digoxin is around 30 minutes, similar to digoxin.
· Digoxin duration of action: The duration of action for digoxin is typically 1 to 4 days.
· Digitoxin duration of action: The duration of action for digitoxin is around 5 to 7 days.
Mechanism of Action of Cardiac Glycosides (digitalis):
The force of cardiac muscle contraction is directly related to the concentration of free calcium ions within the cardiac muscle cells. This intracellular calcium concentration is tightly regulated by several mechanisms, including the sodium-potassium pump and the sodium-calcium exchanger (NCX).
Sodium-Potassium pump: The sodium-potassium pump (Na+/K+ ATPase) maintains the electrochemical gradient across the cell membrane by actively pumping sodium ions (Na+) out of the cell and potassium ions (K+) into the cell. This creates a low sodium concentration inside the cell.
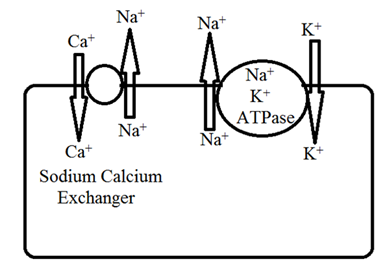
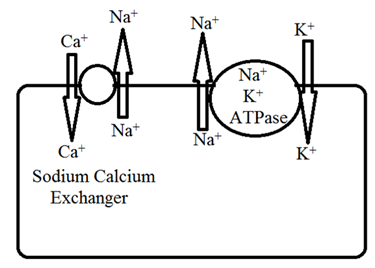
Inhibition of sodium-potassium ATPase: Digitalis exerts its therapeutic effect by binding to and inhibiting the sodium-potassium pump. This inhibition leads to an increase in intracellular sodium concentration.
Indirect increase in intracellular calcium: The sodium-calcium exchanger (NCX) normally utilizes the sodium gradient (high sodium outside, low sodium inside) to remove calcium ions (Ca2+) from the cell in exchange for sodium ions entering. The NCX activity depends on the low intracellular sodium to function efficiently.
The increased intracellular sodium due to digitalis action on the sodium-potassium pump weakens the NCX's ability to remove calcium. Consequently, calcium accumulates inside the cardiac muscle cell.
Increased cardiac contractile force: This elevated intracellular calcium ions concentration has a positive inotropic effect. It increases the force of cardiac muscle contraction. The increased calcium enhances the interaction between the contractile protein actin and myosin, leading to stronger contractions.
Increased Cardiac Output: The stronger contractions increase stroke volume and cardiac output.
Pharmacological Effects of Cardiac Glycosides (Digitalis)
Digitoxin and Digoxin are proto-type drugs under cardiac glycoside. These cardiac glycosides have similar pharmacological effects with variations in the extent of their pharmacological effects.
Cardiovascular system:
a) Positive inotropic effect:
Stronger Heartbeat: Cardiac glycosides (Digitalis) increase the heart ventricles wall contraction force. It modifies the cardiac muscle's electrophysiological properties, affecting the movement of ions like sodium, potassium, and calcium. This is crucial to the therapeutic and toxic effects of digitalis. The positive ionotropic effect of digitalis is dose-dependent.
Filling and Emptying: Cardiac glycosides (Digitalis) help the heart pump more blood with each beat (Increase in cardiac output). It increases the intensity of cardiac muscle contraction and decreases the time to reach the pick of contraction force. The effects on the timing of the heart's contraction and relaxation phases (systole and diastole) provide sufficient time for the complete filling and emptying of the ventricle with blood to increase cardiac output.
Normal vs failing heart: Cardiac glycosides (Digitalis) help both failing and normal hearts beat stronger. However, it has a bigger impact on failing hearts. Failing hearts are often stretched out, and digitalis helps them contract more effectively. The effect is much more pronounced on failing hearts due to the Frank-Starling mechanism. In a normal heart, the heart is already working well, so the extra boost from digitalis may not increase the amount of blood pumped as much.
Oxygen Demand: Even though digitalis makes the heart work harder, it doesn't usually increase the heart's oxygen needs. This is because digitalis improves the calcium utilisation and other factors inside the cells in the heart muscle, making the contractions more efficient.
Digitalis uses: Digitalis is best for hearts that aren't pumping enough blood (heart failure with reduced ejection fraction or HFrEF) and certain irregular heart rhythms (arrhythmias, especially atrial fibrillation). It's not used for conditions where the heart pumping too much blood, like anemia or hyperthyroidism (overactive thyroid). In these cases, digitalis could be harmful.
b) Heart Rate
Cardiac glycosides (Digitalis) produce bradycardia in patients suffering from congestive heart failure. Cardiac glycosides produce a negative chronotropic effect and a positive inotropic effect. Digitalis slows the heart rate primarily through direct stimulation of the vagus nerve. The baroreceptor reflex and modulation of sympathetic activity play a supporting role.
Mechanism of Bradycardia (Slowing of Heart Rate):
Baroreceptor: Cardiac glycosides increase blood circulation and stimulate baroreceptors in the aortic arch and carotid sinus to send more impulses to the cardiovascular centre in the spinal cord. These impulses from baroreceptors reflexly stimulate parasympathetic outflow to produce bradycardia. But it is not the primary mechanism to slow down heart rate by the digitalis.
Sympathetic nervous system modulation: In CHF, the sympathetic nervous system is overactive to increase heart rate. Digitalis indirectly reduces this excessive sympathetic drive by improving heart function and increasing blood circulation. This slows down the heartbeat rate.
Direct Vagal Stimulation: This is the most important mechanism. Digitalis directly stimulates the vagus nerve to carry impulses through nodose ganglia affecting the sinoatrial node (SA Node) to slow the heart rate. This direct vagal effect is the primary reason for the negative chronotropic effect. These effects of cardiac glycosides through arterial baroreceptors and vagal centre stimulation are called the vagal effect of cardiac glycosides.
Atropine and Exercise: Atropine, an anticholinergic drug, blocks the effects of the vagus nerve and can therefore counteract the bradycardia caused by digitalis. Exercise increases sympathetic activity. Thus, it can also reduce the digitalis bradycardia effect.
Digitalis is used to treat heart failure, it can also be used (with careful monitoring) to control heart rate in certain arrhythmias, even in individuals without heart failure.
c) Refractory Period and excitability:
Therapeutic dose: Cardiac glycosides (Digitalis) decrease arterial refractory period under therapeutic dose through vagal effect. This is because the vagus nerve primarily affects the atria and can reduce the duration of the action potential, thus shortening the refractory period.
Overdose: Overdose or large doses of Cardiac glycosides (Digitalis) prolong the refractory period by directly affecting ion channels in cardiac muscle cells involved in repolarization.
Excitability: Therapeutic doses initially increase excitability due to refractory period shortening. The direct effect of high doses leading to refractory period prolongation ultimately decreases excitability.
AV Node and Ventricular Contraction: Cardiac glycosides (Digitalis) through both direct and vagal effects, prolong the effective refractory period of the AV node. This is a crucial mechanism for their use in certain arrhythmias.
Impulse Transmission: By prolonging the AV node's refractory period, cardiac glycosides slow the conduction of impulses from the atria to the ventricles. This is needed in conditions like atrial fibrillation or atrial flutter, where the atria are firing rapidly and irregularly.
Ventricular Rate: Because the AV node acts as a gatekeeper, slowing conduction through it reduces the number of impulses reaching the ventricles. This leads to a decrease in the ventricular contraction rate. This is the therapeutic goal of arrhythmias.
d) Conduction Velocity: Cardiac glycosides (Digitalis) effects on cardiac conduction velocity are complex and dose-dependent.
i. Atria:
Therapeutic/Low Dose: Digitalis primarily increases atrial conduction velocity. This is largely due to increased vagal tone. The vagus nerve releases acetylcholine, which slows the heart rate but enhances conduction in the atria.
Toxic/High Dose: Therapeutic dose increases arterial conduction but very high doses decrease atrial conduction. This is due to the direct effects of the digitalis glycoside on the atrial muscle cells. This effect also happens in the ventricles at high doses.
ii. AV Node:
Both Therapeutic and Toxic Doses: Cardiac glycosides (Digitalis) decrease AV node conduction velocity. The mechanism involves increased vagal tone (at lower doses) and direct effects on the AV node cells (at higher doses). This slowing of AV node conduction leads to heart block (a dangerous slowing or disruption of the electrical signal between the atria and ventricles) at toxic levels.
iii. Ventricles:
Therapeutic/Low Dose: The direct effect of digitalis glycosides on ventricular conduction is minimal at therapeutic levels. The vagal effects are more prominent in the atria and AV node.
Toxic/High Dose: Cardiac glycosides (Digitalis) decrease ventricular conduction velocity. This has a direct effect on the ventricular muscle cells (myocytes). The glycosides interfere with the sodium-potassium pump, leading to changes in ion concentrations that slow the spread of electrical impulses. This slowing can lead to serious arrhythmias (irregular heartbeats).
e) Automaticity: Cardiac glycosides (Digitalis) increase the automaticity of atrial and ventricular muscles that develop extra ectopic beats and trigger dangerous arrhythmia and tachycardia leading to ventricular fibrillation.
Increased Automaticity: Cardiac glycosides (Digitalis) at higher doses increase the automaticity of both atrial and ventricular muscle cells. Automaticity is the ability of cardiac muscle cells to generate action potentials (electrical impulses) without external stimulation. This increased automaticity leads to ectopic beats (extra heartbeats) arising from these cells.
Ectopic Beats: These extra beats can disrupt the heart's normal rhythm. They can occur in the atria or ventricles.
Ventricular Tachycardia: If the ectopic beats originate in the ventricles it leads to ventricular tachycardia. This is a potentially dangerous rhythm where the ventricles beat very quickly.
Ventricular Fibrillation: Ventricular tachycardia degenerates into ventricular fibrillation. This is a life-threatening arrhythmia. In ventricular fibrillation, the ventricles shiver ineffectively instead of pumping blood leading to cardiac arrest.
Blood vessels:
Direct Vasoconstriction
In normal hearts: Cardiac glycosides directly cause vasoconstriction, increasing peripheral vascular resistance. This effect is mediated by the increased intracellular calcium concentration in vascular smooth muscle cells due to the inhibition of the sodium-potassium pump.
Counteracting Effects on Heart Failure
Vagal Effect: In congestive heart failure (CHF), the vasoconstriction induced by cardiac glycosides is often counteracted by an increased vagal tone. This increased vagal activity decreases heart rate. This helps to reduce myocardial oxygen demand and improve cardiac function.
Sodium Pump Effect: The inhibition of the sodium-potassium pump in cardiac muscle cells leads to increased intracellular sodium, which promotes calcium influx via the sodium-calcium exchanger. This increased calcium enhances the force of cardiac contractions (positive inotropic effect), leading to increased cardiac output. The improved cardiac output helps to improve blood circulation and can indirectly reduce peripheral vascular resistance.
Coronary blood flow: Cardiac glycosides improve coronary blood flow.
Blood pressure: In a normal heart digitalis glycosides increase blood pressure but no such effect precipitates in CHF.
ECG: Diminished amplitude of T waves, depressed ST segment, prolonged PR interval, Short QT interval.
Kidney: Digitalis glycosides increase cardiac output and increase renal blood flow, increase parasympathetic outflow, and decrease in sympathetic outflow. All these lead to diuresis in CHF patients. This leads to loss of water and salt and that is treatment of oedema.
CNS: Higher doses cause nausea and vomiting due to stimulation of CTZ. Toxic dose causes hyperpnoea, mental confusion and visual disturbance.
GIT: High dose causes anorexia, diarrhoea, nausea and vomiting.
Alok Bains.
Digitalis toxicity:
Digitalis has a narrow therapeutic index that has a low margin of safety, and high toxicity with occasional fatality. Digitalis toxicity produces cardiac toxicity and extracardiac toxicity. Extracardiac toxicity affects GIT, CNS, Vision and kidney. Diuresis and hypokalemia are the most common toxic effects of digitalis.
1. Cardiac toxicity: Digitalis toxicity develops cardiac arrhythmia. Digitalis partially or completely disturbs AV node impulse conduction. It disturbs the ventricle heartbeat to develop ventricular extra systole bigeminy and trigeminy. This leads to ventricular tachycardia, ventricular fibrillation and death.
Severe bradycardia (slow heart rate), disturbance in arterial rhythm, arterial extra systole, arterial fibrillation, and atrial flutter may appear on digitalis cardiac toxicity due to digitalis's effects on the AV node and sinoatrial (SA) node (the heart's natural pacemaker).
2. GIT: Digitalis glycosides produce gastric irritation, Mesenteric blood vessel constriction and CTZ stimulation. These all lead to anorexia, nausea, vomiting abdominal pain and diarrhoea.
3. CNS: disorientation, confusion, psychosis, aphasia, delirium hallucination along with headache, fatigue and drowsiness. No physical activity, or neuralgic pain.
4. Eye: visual disturbance blurred vision diplopia, amblyopia, colour disturbance.
Treatment:
Stop administration of digitalis glycosides. The body recovers itself from extracellular toxicity by discontinuation of digitalis glycosides administration. In cardiac toxicity, the following measures are adopted
1. Severe tachycardia: Chronic use of digitalis and diuretics may develop hypokalemia and severe tachycardia. In chronic conditions, potassium is administered intravenously and in moderate or mild conditions potassium is administered orally. Acute administration of large doses of digitalis glycosides may develop tachycardia and increased plasma levels of potassium ions. In this condition, potassium ion is not administered
2. AV node impulse conduction block: It can be treated by administering atropine through an intramuscular route.
3. Supraventricular arrhythmia: Lignocaine, phenytoin and potassium salt are administered. Potassium levels in blood plasma and ECG should be closely monitored.
4. Ventricular arrhythmia: Lignocaine, phenytoin and propranolol are used. In life-threatening conditions, antibodies to glycosides are administered.
Alok Bains
Frank-Starling mechanism
The Frank-Starling mechanism, also known as Starling's law of the heart, describes the relationship between the heart's stroke volume (the amount of blood pumped out with each beat) and the end-diastolic volume (the amount of blood in the ventricles just before contraction).
Increased Filling: Increased blood returns to the heart lead to greater end-diastolic volume.
Stretching: This increased volume stretches the heart muscle fibres in the ventricles.
Stronger Contraction: Within a certain physiological range, the more the heart muscle is stretched, the stronger the contraction. This is because the stretching optimizes the overlap of the protein filaments (actin and myosin) within the muscle cells. This allows more forceful cross-bridge formation and contraction.
Increased Stroke Volume: The stronger contraction results in a greater stroke volume, meaning the heart pumps more blood with each beat.
Digitalis and the Frank-Starling Mechanism
Digitalis enhances the Frank-Starling mechanism by increasing the force of ventricle contraction. This means the heart will contract more forcefully and pump more blood.
Clinical Significance
The Frank-Starling mechanism explains the heart's ability to adapt to changing conditions. For example, more blood returns to the heart during exercise. This increases the end-diastolic volume. The Frank-Starling mechanism causes stronger contractions and increased cardiac output to meet the body's increased demands.
Digitalis's enhancement of the Frank-Starling mechanism is important in heart failure. In heart failure, the heart muscle is weakened and may not be able to pump enough blood to meet the body's needs. Digitalis improves cardiac output by increasing the force of contraction for a given end-diastolic volume, even if the heart muscle is weakened.
Important Note: The Frank-Starling mechanism has its limits. Beyond a certain point, excessive stretching of the heart muscle can weaken contractions. This is one of the reasons why it's important to monitor the dose of digitalis carefully and to use it only under the guidance of a healthcare professional. Another reason is digitalis narrow therapeutic index and cumulative effects of digitalis.
Alok Bains
