Hemodynamics
Hemodynamics for MBBS, Nursing and Pharmacy students preparing for university and entrance examinations
PHARMACOLOGY
Alok Singh
2/10/20255 min read
Hemodynamics
“Hemodynamics is the study of blood flow through blood vessels and the forces that affect blood flow.” Blood travels through arteries, arterioles and blood capillaries to deliver oxygen and nutrients to cells. Blood carries carbon dioxide and metabolic wastes from cells through the capillary vein end, venules, vein and venacava to the heart's right atrium.
Factors affecting blood flow: Several factors affect blood flow. Basic: All these factors influence the pressure difference/gradient between two points of blood vessels to force blood flow in blood vessels and cells. Secondarily, blood flow resistance in blood vessels. An increase in pressure difference improves blood flow, and a decrease in blood flow resistance increases blood flow, and vice versa.
Blood Pressure
Mean Arterial Pressure (MAP)
Cardiac Output
Heart Rate
Electric Signal
Nervous System
Stroke volume
Preload
Afterload
Contractility
Venous Return
Muscle Pump
Venous Pump
Respiratory Pump
Zero Pressure
Systemic Vascular Resistance
Blood vessel diameter
Blood Viscosity
Blood Vessel Length
Blood flow velocity
Detail explanation
BLOOD PRESSURE: The pressure exerted by the blood against the inner wall of blood vessels is called blood pressure. It is measured in mm of Hg. Blood pressure is highest in the aorta during cardiac systole. It is systolic blood pressure. Systolic blood pressure falls gradually as blood travels from the aorta to the artery to the arteriole and blood capillaries. Blood pressure is about 120 mm Hg in the aorta, about 110 mm Hg in the artery, about 40 mm Hg in the arteriole and about 30 mm Hg in blood capillaries. Blood pressure falls to about 70 mm Hg during cardiac diastole. It is diastolic blood pressure.
Blood pressure in blood capillaries at the venous end is 18 mm Hg. Blood pressure further falls as blood travels to the right atrium through venules, veins and venacava. Blood pressure is about 16 mm Hg in venules, about 12 mm Hg in veins, about 7 mm Hg in vena cava and zero or negative blood pressure in the right atrium. The pressure differences/pressure gradients influence blood flow in blood vessels from a higher-pressure area to a lower-pressure area.
Mean arterial pressure (MAP): The average blood pressure in the arteries during the cardiac cycle is called mean arterial blood pressure. Formula to calculate MAP
MAP = DP X 1/3 (SP - DP)
SP: Systolic blood pressure
DP: Diastolic blood pressure
MAP = CO X SVR OR, CO = MAP/SVR
CO = Cardiac output
SVR: Systemic Vascular Resistance.
Calculate the MAP of an individual having a blood pressure of 120/80 mm Hg
Ans: MAP = DP X 1/3 (SP - DP)
Where:
Systolic blood pressure (SP) is 120 mm Hg and
Diastolic blood pressure (DP) is 80 mm Hg and
MAP = 120 X 1/3 (120 – 80) = 93 mm Hg
Normal MAP varies from 70 mm Hg to 100 mm Hg.
Cardiac output (CO): The amount of blood the heart pumps per minute is called cardiac output. Formula to calculate Cardiac output:
Cardiac Output (CO):
Heart Rate (HR) X Stroke Volume (SV).
Heart Rate: Number of heartbeats per minute
Stroke volume: The amount of blood the heart pumps per beat.
Mean arterial pressure (MAP) is also used to calculate cardiac output using the formula:
Cardiac Output (CO) = MAP/R
2. HEART RATE: The number of times the heart beats per minute is a heartbeat. The normal resting heart beats 70 to 100 times per minute. Electric signals, hormones and the nervous system control the heart rate.
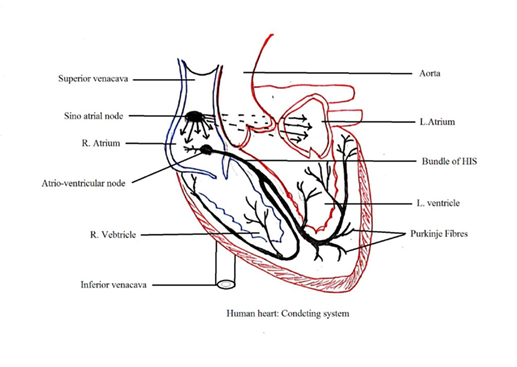
Electric signals: Sinoarterial Node (SA Node) generates electric impulses that travel through a specific pathway to the atrioventricular node (AV Node), the bundle of HIS and Purkinje fibre. The electric signal sets the basic rhythm of the heartbeat.
Nervous system: Under stressful conditions, the sympathetic nervous system stimulates the release of adrenaline and noradrenaline. These hormones activate the SA Node to generate more electric impulses, which accelerates the heart rate. The parasympathetic nervous system stimulates the release of acetylcholine, which decreases the activity of the SA Node to decrease the heart rate.
3. STROKE VOLUME: Stroke volume (SV) is the amount of blood pumped by the heart's left ventricle in one contraction. It determines cardiac output [CO: the blood amount pumped by the heart per minute. CO is calculated by multiplying SV by heart rate (HR): CO = SV x HR]. The following three factors affect the Stroke Volume factors:
a. Preload: The amount of blood in the left ventricle at the end of diastole (the resting phase of the cardiac cycle).
b. Afterload: The resistance to blood flow in the systemic circulation.
c. Contractility: The force of contraction of the left ventricle.
The roles of stroke volume in hemodynamics:
a. Determines cardiac output: Cardiac Output is essential for delivering oxygen and nutrients to the tissues and removing waste products.
b. Affects blood pressure: Stroke Volume affects BP. An increase in Stroke Volume leads to a rise in BP, while a decrease in Stroke Volume leads to a fall in BP.
c Indicator of cardiac function: Stroke Volume is used to assess heart failure and to guide treatment.
4. VENOUS RETURN: Blood flow from the peripheral veins to the right atrium is called venous return. Blood travels towards the right atrium from the lower body part to the right atrium against the gravitational force due to the reasons below.
a. Muscle pump: Rhythmic contraction and relaxation in skeletal muscles surrounding the vein pushes blood towards the heart.
b. Venous valves: Veins have proximal valves closer to the heart and distal valves away from the heart. The two types of valves prevent the backflow of blood in veins and ensure unidirectional blood flow towards the right atrium. Contraction in skeletal muscle surrounds veins compresses the veins and pushes blood flow towards the right atrium by opening the proximal valves. Relaxation in skeletal muscle surrounding the veins closes the distal valves to block the backflow of blood. Skeletal muscle contractions surrounding veins in the legs to push deoxygenated blood towards the heart and venous valves to prevent blood backflow in veins constitute a venous pump. The venous pump acts as a secondary pump to help venous return.
c. Respiratory pump: Rhythmic contraction and relaxation of respiratory muscles during respiration push venous blood in the respiratory area towards the right atrium. The diaphragm moves downward during inhalation decreasing the thoracic cavity pressure and increasing the abdominal cavity pressure. This exerts pressure on the abdominal vein to compress and relax pressure on the vein in the thoracic cavity. Compression of veins in the abdominal cavity and relaxation of veins in the thoracic cavity during inhalation pump blood to flow towards the right atrium. The diaphragm moves upward during exhalation decreasing thoracic cavity pressure and increasing abdominal cavity pressure. This causes blood backflow in the thoracic veins. But valves present in the veins stop the blood backflow.
d. Zero pressure: Zero or negative pressure in the right atrium sucks blood from veins to the right atrium.
5. SYSTEMIC VASCULAR RESISTANCE (SVR) or Peripheral Vascular Resistance (PVR): Resistance to blood flow inside blood vessels is called Systemic Vascular Resistance. Friction between blood and blood vessel wall develops SVR. An increase in SVR decreases the blood flow and a decrease in SVR increases the blood flow. The following factors affect the SVR.
a. Blood vessel diameter: Narrow blood vessel (vasoconstriction) increases the resistance in blood flow. Wide blood vessel (vasodilation) decreases the resistance in blood flow. Thus, SVR is inversely proportional to blood vessel diameter.
b. Blood Viscosity: A high concentration of blood cells and/or plasma protein increases the blood viscosity making blood thicker. This increases the resistance in blood flow inside blood vessels.
c. Blood vessel length: Longer blood vessels have more resistance to blood flow than shorter blood vessels.
6. BLOOD FLOW VELOCITY: The blood vessel cross-section area affects the resistance in flow velocity. Both are inversely proportional to each other. Larger blood vessel cross-section areas slow down blood flow velocity. Branches of arteries form capillaries. The total cross-section area of the blood capillaries shall be higher than the cross-section area of the artery. Thus, the blood flow rate in the capillary bed is slower than in arteries. This slow blood flow promotes gases and nutrient exchange between cells and capillaries. Venules union form veins. The total cross-area of venules shall be greater than the vein. A faster blood flow rate in the vein assists venous return to the heart.
The blood flow rate decreases as it travels from the aorta to arteries to capillaries and the blood flow rate accelerates from venules to vein to vena cava.
ALOK BAINS
