HSBTE DMLT 1st Semester Hematology Question Paper
HSBTE DMLT Hematology, Ist Semester, Sample Paper with Solutions
HSBTE QUESTION SOLUTION
Alok Bains
12/10/202353 min read
HSBTE Sample Paper Hematology, Ist Semester, Questions with Solution
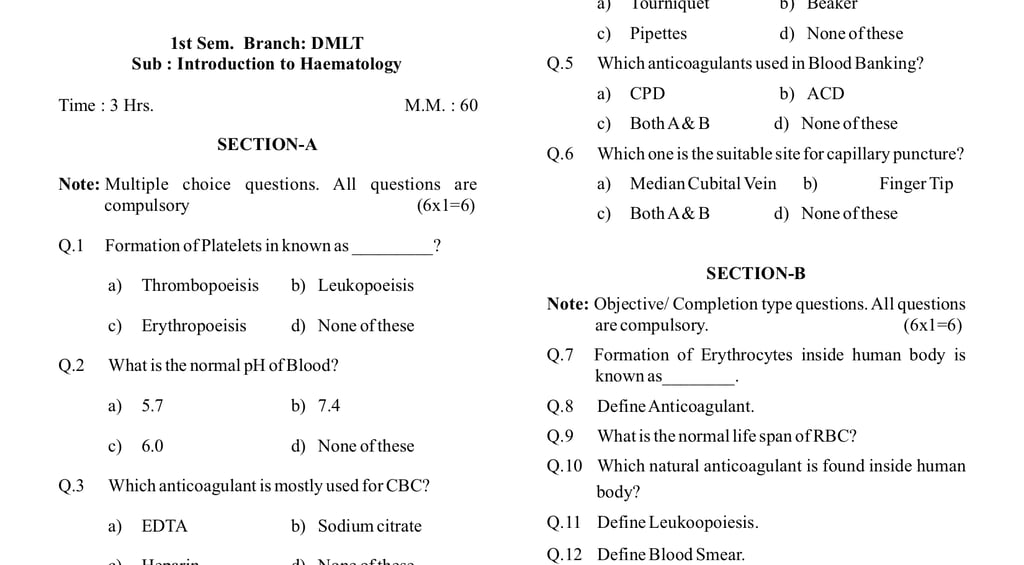
1st Semester, DMLT. Subject: Introduction to Haematology, Code: 221916
Sample 1
Introduction to Haematology, Time : 3 Hrs. M. M.: 6s0
SECTION-A
Note: Multiple-choice questions. All questions are compulsory (6x1=6)
Q.1 Formation of Platelets in known as _________?
a) Thrombopoiesis b) Leukopoiesis c) Erythropoiesis d) None of these.
Ans: a) Thrombopoiesis
Q.2 What is the normal pH of Blood?
a) 5.7 b) 7.4 c) 6.0 d) None of these
Ans: b) 7.4
Q.3 Which anticoagulant is mostly used for CBC?
a) EDTA b) Sodium citrate c) Heparin d) None of these
Ans: a) EDTA
Note: EDTA: Ethylenediamine Tetraacetic Acid. CBC: Complete Blood Coun
Q. 4 Which one is used during venous Blood collection?
a) Tourniquet b) Beaker c) Pipettes d) None of these
Ans: a) Tourniquet
Q.5 Which anticoagulants are used in Blood Banking?
a) CPD b) ACD c) Both A & B d) None of thes
Ans: c) Both A & B
Note: CPD: Citrate Phosphate Dextrose (in solution form). ACD: Acid Citrate Dextrose (in solution form).
Q.6 Which one is the suitable site for capillary puncture?
a) Median Cubital Vein b) Finger Tip c) Both A & B d) None of these
Ans: b) Finger Tip
Note: The middle or Ring fingertip of the non-dominant hand is used for capillary puncture because they are less sensitive to pain. They are also less calloused than the thumb and index finger. The thumb is also avoided due to the presence of more arteries in the thumb
SECTION-B
Note: Objective/ Completion type questions. All questions are compulsory. (6x1=6)
Q.7 Formation of Erythrocytes inside the human body is known as________.
Ans: Erythropoiesis.
Note: Erythropoiesis occurs in the bone marrow.
Q.8 Define Anticoagulant.
Ans: An anticoagulant is a substance that prevents blood from clotting or reduces the formation of blood clots. Examples are Heparin, EDTA, CPD, ACD, etc. Heparin is a natural coagulant present in human blood inside the human body's blood Vessels.
Q.9 What is the normal life span of RBC
Ans: 120 days.
Q.10 Which natural anticoagulant is found inside the human body?
Ans: Hepari
Q.11 Define Leukoopoiesis
Ans: The process of white blood cell (leukocyte) formation or production in the body is called Leukopoiesis.
Note: Leukopoiesis is a part of hematopoiesis. The overall process of forming blood cells is called hematopoiesis
Q.12 Define Blood Smear.
Ans: Blood smear is a laboratory technique to form a thin layer of blood on a microscope slide.
Note: A blood smear is also known as a peripheral blood smear or peripheral blood film. The blood smear provides detailed information about the cellular components of blood, including red blood cells (erythrocytes), white blood cells (leukocytes), and platelets.
SECTION-C
Note: Short answer type questions. Attempt any eight questions out of ten questions. (8x4=32)
Q.13 Write the various functions of blood.
Ans: Blood is composed of plasma and blood cells. Each component performs its functions.
A. Plasma Proteins Functions: Blood plasma has several proteins. These proteins transport absorbed food, respiratory gases, metabolic wastes, hormones, antibodies, heat, clotting factors, etc.
B. Function of Red Blood Cells (Erythrocytes): RBC contains hemoglobin that transports respiratory gases and maintains blood pH.
C. Function of White Blood Cells (Leucocytes): Protection of the body from microorganisms and toxins produced by the microorganism.
D. Function of blood platelets: They help in blood coagulation and clot formation.
Q.14 Draw and write the uses of Hb. RBC and WBC Pipette.
Ans: Hemoglobin (Hb) pipette, Red Blood Cell (RBC) pipette, and White Blood Cell (WBC) pipette are laboratory instruments used in hematology for the measurement and analysis of blood components.
A. Hemoglobin (Hb) Pipette
Hemoglobin Pipette is used for the collection of blood from capillary puncture for hemoglobin estimation. It has a single mark of 20 cu mm.
B. Red Blood Cell (RBC) Pipette
C. The RBC pipette is a diluting pipette. The RBC pipette is used to dilute blood samples for RBC count in the Hemocytometer. RBC pipette has a red bead in the bulb and it has markings of 0.5, 1, and 101. Red bead helps in the mixing of diluting fluid and blood.
D. White Blood Cell (WBC) Pipette
WBC pipette is a diluting pipette. The WBC pipette is used to dilute blood sample for RWBC count in the Hemocytometer.
Q.15 Define Plasma and write their compositions.
Ans: Definition: Blood plasma is the yellowish liquid component of blood that contains soluble components of blood and suspended blood cells. Blood plasma constitutes 55% of the total blood volume.
Composition of blood plasma: It consists of the following componenets
A. Water: Approximately 90-92% of blood plasma volume is water.
B. Proteins: Albumin, Globulin, Fibrinogen, etc.
C. Electrolytes: Sodium, Potassium, Calcium, Chloride, etc.
D. Gases: Oxygen, carbon dioxide, etc.
E. Nutrient: Glucose, amino acids, fatty acids, etc.
F. Hormones,
G. Waste Products: Urea, Creatinine, and other metabolic wastes.
Q.16 Describe Non-Calcium chelators anticoagulants.
Ans: Anticoagulants are substances that prevent blood from clotting. Non-calcium chelators and anticoagulants act independently without involving calcium ions in the blood. The following two are commonly used non-chelator anticoagulants
1. Heparin: Heparin is a natural anticoagulant that combines with antithrombin III and catalyzes antithrombin-III ability to inactivate thrombin and other clotting factors.
2. Argatroban: It is a direct thrombin inhibitor. It does not require antithrombin III for its anticoagulant effect
Q17 Describe the selection and preparing of the vein puncture site.
Ans: SELECTION AND PREPARING OF VENIPUNCTURE SITE
Selection of site for venipuncture: The following veins are suitable for venipuncture.
Inside antecubital fossa located in the elbow
a. Cephalic vein: The cephalic vein runs an entire arm's length.
b. Basilic vein: A basilic vein is a vein located in the triangular area inside the elbow. The basilic vein is considered an alternate site for venipuncture. It is used if other more prominent arm vein is not visible.
c. Median cubital vein: The median cubital vein connects the cephalic vein and basilic vein. It is preferred due to its large size and lower tendency to roll during needle insertion. Very few nerve endings surround this vein. Thus it is less painful to insert the needle into a median cubital vein.
These three veins are superficially located in the triangular area inside the elbow.
d. Superficial veins in foot and ankle
The median cubital vein and cephalic vein near the median cubital vein are the most common and suitable sites for vein puncture. Sometimes hand vein is selected if these three veins are not prominent. Hand veins tend to roll. Thus the skin is pulled taut then a needle is inserted. Superficial veins in the foot and ankle are considered the last alternate site for venipuncture. However, the following sites (areas) should be avoided for venipuncture.
a. Site having scars due to burning or surgery. It is difficult to puncture scar tissue.
b. Mastectomy site. This area has lymphodema. That affects the blood sample test result.
c. Bad bruise (Haematoma) on the skin,
d. Skin part used for intravenous therapy or blood transfusion.
e. Skin with an infection like eczema or any other disease condition.
f. Arm with canula or fistula or heparin leak. This site should be used only after physician consultation.
g. Endematous extremities. This area has tissue fluid accumulation. These fluids may enter blood samples. That will dilute blood and affect blood test reports.
h.Thrombosed vein.
Preparation for venipuncture: Select the venipuncture exact site by tracing the palpating vein using the index finger. If palpitation is not felt easily then the following measures are taken to improve blood flow towards the venipuncture site
i. The arm is massaged from the wrist to the triangular inner side of the elbow.
ii. Tap the venipuncture site by using the index finger and middle finger.
iii. Apply a warm moist cloth to the venipuncture site at least for 5 minutes,
iv. Lowering of the arm below bed level also allows the vein to be filled with venous blood.
Q.18 Write the materials and equipment required for capillary puncture.
Ans: MATERIALS AND EQUIPMENTS REQUIRED FOR CAPILLARY PUNCTURE SITE:
Capillary punctures require different devices such as lancets, microcontainer tubes, microhematocrit tubes, sealants, alcohol (ethyl alcohol or isopropyl) as a disinfectant, and warming devices. Improper use of these devices may cause improper specimen collection and pre-analytical errors.
i. Lancets are meant to puncture or cut the skin to collect capillary blood. They are specifically designed for finger or heel puncture.
ii. Microcontainer tubes is used to collect minute volumes of blood via capillary puncture. They are coated with different additives.Colour code on microcontainer tube represents the additive present inside it. They have also markings indicating the volume in µL.
iii. Microhematocrit tubes are glass or plastic capillary tubes. They are used for blood collection and hematocrit determination. They are either coated with anticoagulant or plain. Plastic or clay sealants are commonly used. It makes Microhematocrit tubes leak-proof seal.
iv. Warming device (heel warmer): It is used to increase the arterial blood flow at the puncture site. It makes a close resemblance of sample blood with arterial blood to venous blood. A towel dampened with warm water can be used to produce the same effect as a warming device. However, water should not be too hot to burn the patient.
Q.19 Describe the Vacutainer system in brief.
Ans: VACUTAINER SYSTEM: It is also known as an evacuated collection tube. It is made up of glass or plastic. If an additive is present in the collection tube then it is called an additive collection tube. If the collection tube has no additive then it is called a non-additive collection tube. The collection tube has a colored rubber or plastic top (colored rubber or plastic stopper). This color is used to indicate the specific hematological test to be performed by using blood present in the collection tube. This color also indicates the additives added to the collection tube.
A sterilized collection tube (vacutainer) is used to collect and store blood from the vein of the patient. The sterilized top of the collection tube is inserted into a connector attached to a butterfly needle. The tube is further pushed into the connector. This creates a vacuum in a sterilized collection tube. The top of the needle is pierced into a vein of the patient. Blood automatically enters into a sterilized collection tube due to the vacuum created by the collection tube.
A collection tube (vacutainer) is a closed system to withdraw blood from a vein through a venipuncture procedure. This prevents exposure of blood to air or outside contaminants. It is available in various sizes and volumes. This size is selected as per requirements such as the age of the patient, volume of blood to be collected, condition of the patient’s vein, and size of the patient’s vein.
Each collection tube has an expiry date that is for the additive and vacuum system of the collection tube. The collection tube should be filled properly. Improper filling shall disturb blood and additive proportion (ratio). This will not give accurate test results. This type of sample shall also be rejected by a laboratory technician.
Q.20 Write the procedure of preparation of Thick blood film.
Ans: A thick blood film is commonly used in the diagnosis of malaria and other bloodborne parasites.
Procedure:
1. Prepare the Patient: Explain the procedure to the patient and obtain informed consent. Select a suitable site for blood collection (commonly the fingertip or earlobe), Clean the selected site with an alcohol swab.
2. Collect Blood: Use a lancet or needle to puncture the cleaned site and collect a small drop of blood on one end of the clean microscopic slide.
3. Make a Thick Blood Smear: Spread the blood in a circular motion to create a thick and even film by using a spreader slide. The size of the smear should be about the diameter of a dime or slightly larger.
4. Allow the Blood Smear to Air-Dry: Allow the thick blood smear to air-dry completely. This can take several minutes.
5. Fix the Blood Smear: Fix the blood smear by immersing the slide in methanol or other fixative for 1-2 minutes. This step helps in preserving the cellular morphology.
6. Rinse and Dry: Rinse the stained slide with distilled water to remove excess stain. Allow the slide to air-dry completely.
Q.21 Describe the Romanowsky stain in brief.
Ans: Romanowsky stains are a group of histological stains used in microscopy to color and differentiate various components of cells. These stains are commonly employed in hematology for the microscopic examination of blood cells and blood-borne parasites. One of the most well-known Romanowsky stains is Giemsa stain, which is widely used for staining blood smears in the diagnosis of malaria and other blood-related disorders,
Romanowsky stain consists of water-soluble eosin, methylene blue, and acetone-free methanol.
1. Eosin is an anionic acidic dye that imparts pink and red color to cellular structure. Eosin combines with cationic components of cells eg Cytoplasm.
2. Methylene blue is a cationic basic dye that imparts blue-purple colour to cellular structure. Methylene blue combines with an anionic component of cells eg DNA.
3. Acetone is a strong decolourising agent and a strong dehydrating agent. Thus acetone-free methanol (Absolute methanol) is used as an ingredient in the Romanowsky stain. This acetone will destroy the cell membrane. Methanol acts as a fixative.
Pink-red or deep red color Red blood cells.
Gray-blue color: Reticulocytes.
Pale pink cytoplasm, purple granule Neutrophil
Pale pink cytoplasm, Eosinophil
Blue cytoplasm, Dark blue Basophil
Blue cytoplasm Monocytes
Dark blue cytoplasm Lymphocyte
Purple color Platelets
Bluish purple RNA, DNA.
Q.22 Describe Thrombopoiesis in brief.
Ans: Thrombopoiesis is the process of platelets (thrombocytes) formation. It is a part of hematopoiesis (the formation of blood cells). Thrombopoiesis occurs in the bone marrow. It involves a series of steps to produce mature platelets.
1. Hematopoietic Stem Cells: Thrombopoiesis begins with hematopoietic stem cells (HSCs) in the red bone marrow. Megakaryocytes of stem cells develop platelets. One megakaryocyte develops 1000 platelets. Hormone thrombopoietin stimulates the production of platelets.
2. Megakaryocyte Maturation: Megakaryocytes are large, multinucleated cells. They undergo maturation within the red bone marrow. They develop a complex cytoplasmic structure with multiple lobes. These are mature Megakaryocytes (Proplatelets).
3. These mature Megakaryocytes undergo fragmentation and form small platelets.
4. The newly formed platelets are released into the bloodstream from the bone marrow.
5. Platelets Lifespan: Platelets have a relatively short lifespan about 7-10 days.
SECTION-D
Note: Long answer type questions. Attempt any two questions out of three questions. (2x8=16)
Q.23 Describe the development stages of the Erythrocyte in detail.
Q.24 Explain various anticoagulant vials/tubes with their color code and uses.
Q.25 Explain the Requirement, Preparation, and procedure for capillary blood collection.
Dr Pramila Singh
SAMPLE 2
1st Year / DMLT, DMLT Subject: Introduction to Haematology Time: 3 Hrs. M.M.: 60
SECTION-A
Note: Multiple-choice questions. All questions are compulsory (6x1=6)
Q.1 The study of blood and its components is called
a) Haematology b) Microbiology c) Histology d) None of these
Q.2 For coagulation studies, the ratio of blood to anticoagulant is
a) 9:1 b) 7:1 c) 8:1 d) None
Q.3 Which one is a natural anticoagulant found inside the human body?
a) EDTA b) Sodium citrate c) Heparin d) None of these
Q.4 Which one is used during Venous Blood collection?
a) Tourniquet b) Beaker c) Pipettes d) None of these
Q.5 Which one is used to puncture the skin to collect capillary Blood?
a) Needles b) Lancet c) Both A & B d) None of these
Q.6 Which one acts as a Fixative in the staining solution?
a) Azure b) H & E c) Eosion d) None of these.
(Hematoxylin & Eosin stain; Hematoxylin acts as a fixative component).
SECTION-B
Note: Objective/ Completion type questions. All questions are compulsory. (6x1=6)
Q.7 The Formation of erythrocytes inside the human body is known as …..
Ans: Erythropoiesis
Q.8 Expand EDTA & ACD.
EDTA → Ethylene Diamine Tetraacetic Acid, ACD → Acid Citrate Dextrose
Q.9 Define the term Vacutainer?
A Vacutainer is a sterile glass or plastic tube with a colored stopper. It creates a vacuum inside the tube to draw a predetermined volume of blood. It is commonly used in blood collection for laboratory tests.
Q.10 Which anticoagulant is mostly used for CBC?
EDTA (Ethylenediamine Tetraacetic Acid) is the anticoagulant most commonly used for Complete Blood Count (CBC).
Q.11 Define Thrombopoiesis.
Thrombopoiesis is the biological process of platelet (thrombocytes) formation from megakaryocytes in the bone marrow.
Q.12 What is capillary blood?
Capillary blood is the blood obtained from the capillaries through a finger prick, heel prick, or ear lobe puncture. It is a mixture of arterial, venous, and interstitial fluids. It is commonly used for blood glucose and other rapid tests.
SECTION-C
Note: Short answer type questions. Attempt any eight questions out of the ten questions. (8x4=32)
Q.13 Write the various functions of blood.
Functions of Blood
Transport – Carries oxygen, carbon dioxide, nutrients, hormones, and waste products.
Regulation – Maintains pH, body temperature, and water balance.
Protection – Provides immunity through WBCs and antibodies; clotting prevents blood loss.
Homeostasis – Maintains internal stability of the body.
Storage – Stores nutrients, iron, and other substances in plasma.
Q.14 Write the uses of the RBC and WBC Pipette.
Uses of the RBC and WBC Pipette
RBC Pipette
Used to dilute blood for counting red blood cells.
Marked at 0.5, 1.0, and 101 to give a dilution ratio of 1:200.
WBC Pipette
Used to dilute blood for counting white blood cells.
Marked at 0.5, 1.0, and 11 to give a dilution ratio of 1:20.
Q.15 Define Plasma and write three compositions.
Plasma: The clear, straw-colored liquid portion of blood that remains after removal of blood cells. It makes up 55% of the total blood volume.
Main Compositions:
Water (~90–92%)
Plasma Proteins (albumin, globulin, fibrinogen)
Solutes (glucose, electrolytes, gases, hormones, metabolic wastes)
Q.16 Describe Non-calcium chelators anticoagulants.
Non-calcium Chelators Anticoagulants
These anticoagulants do not act by binding calcium. They inhibit clotting through other mechanisms. Examples:
Heparin – Acts by potentiating antithrombin III, preventing fibrin formation.
Direct Thrombin Inhibitors (DTIs) – Block thrombin activity directly.
Direct Factor Xa Inhibitors – Prevent prothrombin activation. Used in hematology and clinical chemistry tests.
Q.17 Describe the selection and preparation of the puncture site.
Selection and Preparation of the Puncture Site
Selection:
Common sites: ring finger, middle finger (adults); heel (infants).
The chosen site should be warm, free from scars, swelling, or infection.
Preparation:
1. Clean the puncture site with a 70% alcohol swab.
2. Allow to air-dry to avoid hemolysis.
3. Perform a puncture with a sterile lancet at the side of the fingertip/heel.
Q.18 Write the materials & equipment required for capillary puncture.
Materials & Equipment Required for Capillary Puncture
Sterile lancets
Alcohol swabs (70% ethanol)
Cotton/gauze pads
Capillary tubes or micropipettes
Antiseptic solution
Gloves and protective equipment
Small bandage/plaster
Q.19 Describe the Vacutainer system in brief.
Closed blood collection system using a double-ended needle, plastic holder, and evacuated tubes with pre-measured vacuum.
Advantages:
Reduces contamination and exposure to blood.
Collects multiple samples without repeated punctures.
Tubes contain pre-added anticoagulants or clot activators.
Q.20 Write the procedure for the preparation of a thick blood film.
i. Place a large drop of blood in the center of a clean slide.
ii. Spread gently with the corner of another slide in a circular motion.
iii. Make a thick, even film about 1 cm in diameter.
iv. Air-dry (do not fix in methanol, unlike thin film).
v. Stain with Romanowsky stain for malaria parasite detection.
Q.21 Describe Romanowsky stain in brief.
Romanowsky Stain
A group of polychromatic stains (e.g., Leishman, Giemsa, Wright’s) used in hematology.
Principle: A Combination of acidic dye (eosin) and basic dye (methylene blue/azure) produces multiple staining effects.
Uses:
Staining blood films for differential leukocyte count.
Identifying blood parasites (e.g., malaria).
Q.22 Describe Thrombopoiesis in brief.
Thrombopoiesis
Definition: The process of platelet (thrombocyte) formation from bone marrow.
Steps:
Hematopoietic stem cell → Megakaryoblast → Megakaryocyte.
Megakaryocytes release cytoplasmic fragments (platelets) into circulation.
Regulation: Controlled by Thrombopoietin (TPO) produced in the liver and kidney.
Normal count: 1.5–4.5 lakhs/µL of blood.
SECTION-D
Note: Long answer type questions. Attempt any two questions out of the three questions. (2x8=16)
Q.23 Describe the preservation and disposal of processed blood samples.
Preservation of Processed Blood Samples
Refrigeration (2–8 °C):
Whole blood and serum samples are kept in the refrigerator for short-term storage (hours to a few days).
Prevents bacterial growth and degradation of components.
Freezing (−20 °C or −80 °C):
Plasma and serum can be frozen for long-term storage.
Maintains stability of proteins, enzymes, and metabolites.
Use of Preservatives/Anticoagulants:
EDTA, heparin, citrate, or oxalate are added to prevent clotting, depending on test requirements.
Proper Labelling:
Each sample should be labelled with patient details, date, and type of preservative used.
Sealed Containers:
Blood products are stored in sterile, leak-proof, and closed containers to avoid contamination.
Disposal of Processed Blood Samples
Biohazard Safety Rules:
Treated as bio-medical waste under biomedical waste management guidelines.
Collection:
Disposed of in yellow-colored biohazard bags/containers (for infectious waste).
Disinfection:
Autoclaving or chemical treatment (e.g., 1% sodium hypochlorite for at least 30 minutes) before disposal.
Incineration/Deep Burial:
Final disposal by incineration (burning at high temperature) or deep burial in approved sites.
Sharps (needles, glass):
Collected separately in puncture-proof containers before treatment and disposal.
Preserve by refrigeration, freezing, or with anticoagulants in labelled, sterile containers.
Dispose of by autoclaving/disinfection, then incineration or burial as per biomedical waste rules.
Q.24 Explain the Requirement Principle and procedure for venous blood.
Venous Blood Collection
Principle:
Venous blood is collected by venipuncture, which involves puncturing a vein (usually in the arm) to obtain blood.
The principle is to access the vein safely with minimal trauma, using sterile equipment, so that blood remains uncontaminated and suitable for diagnostic tests.
It ensures adequate volume for hematology, biochemistry, serology, and microbiology investigations.
Requirements (Materials):
Personal protective equipment (PPE): Gloves, lab coat, mask.
Tourniquet: To make the vein more prominent.
Sterile needles: Single-use (21–23 gauge for adults, 23–25 for children).
Syringe or vacuum collection system (e.g., vacutainer).
Alcohol swabs/antiseptic solution (70% isopropyl alcohol).
Collection tubes: Depending on the test (EDTA, citrate, heparin, plain).
Cotton swabs/gauze: To stop bleeding after a puncture.
Plaster or bandage.
Sharps container: For safe disposal of used needles.
Properly labeled request form and labels for samples.
Procedure of Venous Blood Collection
Preparation:
Wash hands and wear gloves.
Verify patient identity and explain the procedure.
Position the patient comfortably (sitting or lying down).
Site selection:
Common sites: median cubital vein (preferred), cephalic vein, basilic vein.
Apply a tourniquet about 3–4 inches above the site to engorge the vein.
Skin antisepsis:
Clean the puncture site with 70% alcohol in a circular motion (inside to outside).
Allow the area to dry.
Venipuncture:
Hold the vein steady with the non-dominant hand.
Insert the sterile needle bevel-up at about a 15–30° angle into the vein.
Once in the vein, blood will flashback into the hub.
Collection:
Attach syringe or vacutainer tube to collect the required amount of blood.
If multiple tubes are needed, follow the order of draw (e.g., blood culture → citrate → serum → heparin → EDTA → fluoride).
Completion:
Release the tourniquet before withdrawing the needle.
Withdraw the needle gently and apply sterile gauze or cotton over the site.
Ask the patient to press and hold for 2–3 minutes.
Apply a bandage if necessary.
Post-collection:
Transfer blood to the correct tubes (if using a syringe).
Mix anticoagulant tubes gently by inversion (do not shake).
Label the tubes with patient details immediately.
Aftercare & disposal:
Dispose of the needle in a sharps container.
Remove gloves and wash hands.
Ensure patient comfort and check for bleeding or hematoma.
Caution:
Always maintain aseptic technique.
Do not leave the tourniquet on for more than 1 minute (to avoid hemoconcentration).
Never recap used needles.
Ensure correct labeling to avoid sample mix-ups.
Q.25 Explain various anticoagulant vials/tubes with their color code and uses.
Anticoagulant Tubes: Color Codes and Uses
Anticoagulant tubes contain chemicals that prevent blood clotting. They are color-coded for easy identification in phlebotomy and laboratory use.
1. Purple/Lavender Top – EDTA (Ethylenediaminetetraacetic acid)
Anticoagulant: EDTA (binds calcium → prevents clotting)
Uses:
Hematology tests (CBC, ESR, peripheral smear)
Blood typing and cross-matching
Note: Preserves cell morphology best.
2. Light Blue Top – Sodium Citrate
Anticoagulant: Sodium citrate (binds calcium reversibly)
Uses:
Coagulation studies (PT, aPTT, INR, D-dimer, fibrinogen)
Platelet function tests
Note: Ratio of blood:anticoagulant must be 9:1 for accuracy.
3. Green Top – Heparin (Lithium/Sodium/Ammonium Heparin)
Anticoagulant: Heparin (inhibits thrombin and clotting factors)
Uses:
Plasma chemistry tests (electrolytes, enzymes, hormones)
Blood gas analysis
Note: Preferred when rapid analysis is needed; avoids clotting artifacts.
4. Gray Top – Potassium Oxalate + Sodium Fluoride
Anticoagulant: Potassium oxalate (binds calcium)
Additive: Sodium fluoride (glycolysis inhibitor)
Uses:
Glucose testing (blood sugar, GTT)
Lactate measurement
Note: Prevents false low glucose values by inhibiting glycolysis.
5. Yellow Top – Sodium Polyanethol Sulfonate (SPS) / ACD (Acid Citrate Dextrose)
Anticoagulant:
SPS: For blood culture bottles (inhibits complement & phagocytes).
ACD: For HLA typing, DNA studies, and transfusion medicine.
Uses:
Microbiology (blood cultures)
Immunohematology and genetic studies
6. Black Top – Sodium Citrate (Buffered, different concentration)
Anticoagulant: Sodium citrate (special ratio for ESR).
Uses:
Westergren ESR (Erythrocyte Sedimentation Rate).
7. Pink Top – EDTA (Spray-coated)
Anticoagulant: EDTA, like lavender.
Uses:
Blood bank testing (crossmatch, antibody screening).
8. Royal Blue Top – EDTA / Heparin / None (Depends on label)
Anticoagulant: EDTA or Heparin (trace element–free tubes).
Uses:
Trace element studies (zinc, copper, lead, heavy metals).
Toxicology studies.
9. White Top (Pearl Cap) – K2EDTA + Gel Separator
Anticoagulant: K2EDTA with gel.
Uses:
Molecular diagnostics (PCR, viral load studied
Dr Pramila Singh
SAMPLE 3
1st Sem / DMLT, Introduction to Haematology Time : 3 Hrs. M.M.: 60
SECTION-A
Note: Multiple-choice questions. All questions are compulsory (6x1=6)
Q.1 Which is a natural anticoagulant?
a) EDTA b) Sodium citrate c) Heparin d) None of these
Q.2 Formation of erythrocytes is known as?
a) Thrombopoiesis b) Erythropoeisis c) Leukopoeisis d) None of these
Q.3 Which anticoagulants are used in Blood Banking?
a) CPD b) ACD c) Both A&B d) None of these
Q.4 Which one is the suitable site for venous puncture?
a) Median Cubital Vein b) Finger Tip c) Both A&B d) None of these
Q.5 Which one of the following is not a Romanowsky stain?
a) Leishman b) Giemsa c) Wright d) Supravital
Q.6 RBC diluting fluid?
a) Hayem's diluting fluid b) Crower's diluting fluid c) Both d) None
SECTION-B
Note: Objective/ Completion type questions. All questions are compulsory. (6x1=6)
Q.7 Formation of WBC inside the human body is known as___________.
Ans Leucopoiesis
Q.8 Define Anticoagulant.
An anticoagulant is a substance that prevents blood clotting by inhibiting the coagulation process. They keep blood in a fluid state.
Q.9 Needle size of___________for adults and ________ for children is used for blood collection.
Ans: Adults → 21–22 gauge Children → 23–25 gauge
Q.10 The recommended location for blood collection for a newborn baby is_____________.
Ans: Heel prick (heel puncture, usually lateral or medial plantar surface of heel)
Q.11 Define Haematology.
Haematology is the branch of medical science that deals with the study of blood, blood-forming organs, and blood-related diseases.
Q.12 Blood is a ________tissue.
Ans: Connective tissue
SECTION-C
Note: Short answer type questions. Attempt any eight questions out of the ten questions. (8x4=32)
Q.13 Describe the procedure for the capillary puncture site.
Procedure for Capillary Puncture Site
1. Preparation
Explain the procedure to the patient to reduce anxiety.
Wash your hands thoroughly and wear gloves.
Select the site: usually the ring or middle finger of the non-dominant hand for adults, or the heel for infants. Avoid fingers with scars, bruises, or edema.
2. Cleaning the Site
Clean the selected site with 70% isopropyl alcohol using a circular motion from the center outward.
Allow it to air dry completely to prevent hemolysis of blood or contamination.
3. Puncturing the Site
Use a sterile lancet appropriate for the patient’s age and the volume of blood needed.
Position the lancet perpendicular to the finger or heel surface.
Puncture swiftly to minimize discomfort.
4. Collecting the Blood
Wipe away the first drop of blood with sterile gauze to remove tissue fluid.
Collect subsequent drops in a capillary tube or directly on test strips, slides, or microcontainers.
Gently massage or milk the finger from base to tip; avoid squeezing excessively, which can hemolyze the blood.
5. After Collection
Apply a sterile gauze pad or cotton ball to the puncture site.
Apply gentle pressure until bleeding stops.
Bandage the site if needed.
6. Disposal
Dispose of the lancet in a sharps container.
Dispose of any contaminated materials according to laboratory biohazard protocols.
7. Documentation
Label the sample accurately with patient details, date, and time.
Record any complications that occurred during the procedure.
Points to Remember
Always use a new sterile lancet for each patient.
Avoid puncturing thumbs or index fingers (more nerve endings).
Ensure proper warming of the site if blood flow is slow (especially in infants or cold hands).
Q.14 Describe the Vacutainer system in brief.
The Vacutainer system is a closed blood collection system widely used in medical laboratories for safe and efficient blood collection. Here’s a brief description:
Components:
Vacutainer tube: A sterile, vacuum-sealed tube with or without additives (anticoagulants, preservatives, or clot activators).
Double-ended needle: One end punctures the vein; the other pierces the tube’s rubber stopper.
Holder or adapter: A plastic sleeve that holds the needle and tube together.
Working principle:
The tube’s vacuum draws blood automatically into the tube when the needle is inserted into the vein.
The type of tube used depends on the test required (e.g., EDTA for hematology, serum separator for chemistry).
Advantages:
Minimizes exposure to blood, reducing infection risk.
Accurate blood volume collection due to vacuum control.
Multiple tubes can be filled from a single venipuncture.
In short, the Vacutainer system is a safe, efficient, and standardized method for blood collection in clinical laboratories.
Q.15 Write the materials and equipment required for vein puncture.
List of materials and equipment required for vein puncture (phlebotomy):
1. Personal Protective Equipment (PPE)
Gloves (disposable, non-sterile)
Lab coat or gown
Face mask (if needed)
Safety goggles (optional, for risk of splashes)
2. Patient Preparation Materials
Alcohol swabs (70% isopropyl alcohol) or antiseptic wipes
Cotton balls or gauze pads
Tourniquet
Adhesive bandages or tape
3. Blood Collection Equipment
Needles (appropriate gauge, usually 21–23G for adults)
Vacutainer or syringe (depending on method)
Needle holder or winged infusion set (“butterfly” needle)
Blood collection tubes (with appropriate anticoagulants or additives)
Tube labels
4. Miscellaneous
Sharps disposal container
Biohazard waste bag
Trash bin
Hand sanitizer
Note: All equipment should be sterile and single-use wherever applicable to prevent infection.
Q.16 Write the procedure for the preparation of a thin blood film.
A thin blood film is commonly used in medical laboratories for microscopic examination of blood cells:
Materials Required
Clean glass slides
Capillary pipette or dropper
Microscope
Staining reagents (e.g., Leishman, Giemsa stain)
Immersion oil (if required)
Procedure
Clean the slide
Ensure the glass slide is free from grease or dust. Use alcohol to clean if necessary and let it dry.
Place a drop of blood
Take a small drop of blood (usually from a finger prick or venous sample) using a capillary tube or pipette.
Place the drop near one end of the slide (about 1 cm from the edge).
Spread the blood
Take a second clean slide (spreader slide).
Hold it at a 30–45° angle to the first slide.
Touch the drop of blood with the edge of the spreader slide to allow the blood to spread along the edge.
Prepare the thin film
Push the spreader slide smoothly and quickly forward along the length of the first slide.
This will create a thin, even film of blood that tapers toward the end.
Air-dry the slide
Allow the thin blood film to air-dry completely.
Do not blow on it or use heat, as this can damage the cells.
Fix the film (if required)
For staining with Romanowsky-type stains (e.g., Giemsa, Leishman), methanol fixation is recommended.
Immerse or flood the dried slide with methanol for 1–2 minutes, then let it dry.
Stain the film
Apply the chosen stain according to the protocol.
After staining, rinse gently with buffered water and allow to air-dry.
Examine under the microscope
Place a drop of immersion oil (for 100x objective) if required.
Examine under the microscope for morphology, parasite detection, or other cellular details.
Tips for a Good Thin Film
The film should be feathered at the tail end (thin edge).
Avoid thick or uneven films; they make microscopic examination difficult.
Work quickly to prevent clotting.
Q.17 Describe Giemsa stain in brief
Giemsa stain is a differential stain commonly used in microbiology and hematology. It is a mixture of methylene blue, eosin, and Azure B dyes.
Purpose: Stains blood smears, bone marrow, and parasites like Plasmodium (malaria) and Trypanosoma.
Mechanism: The dye binds to nucleic acids, staining nuclei dark blue to violet, cytoplasm pale blue, and red blood cells pink.
Applications:
Identification of blood cell morphology.
Detection of malaria parasites and other blood-borne parasites.
Cytogenetics: used for chromosome banding (G-banding).
In short, Giemsa stain is a versatile stain for visualizing cellular and parasitic structures under a microscope.
Q.18 Describe EDTA with its merits and demerits.
EDTA (Ethylenediaminetetraacetic acid)
Definition:
EDTA is a chelating agent that binds to metal ions such as calcium (Ca²⁺), magnesium (Mg²⁺), and iron (Fe³⁺) to form stable, water-soluble complexes. It is widely used in medicine, biochemistry, and laboratory procedures to prevent blood clotting and metal ion interference.
Chemical Formula: C₁₀H₁₆N₂O₈
Mechanism:
EDTA has multiple carboxyl (-COOH) and amine (-NH₂) groups.
These groups bind (chelate) divalent and trivalent metal ions.
In blood, EDTA binds calcium, which is essential for coagulation, thus preventing clotting.
Merits (Advantages) of EDTA
Effective Anticoagulant:
Prevents blood clotting efficiently by chelating calcium ions.
Stable and Safe:
Non-toxic at standard laboratory concentrations.
Preserves Cellular Components:
Maintains the morphology of blood cells for hematological studies.
Versatile:
Used in various fields:
Clinical labs (blood collection, hematology tests)
Molecular biology (prevents metal-induced enzyme degradation)
Industrial processes (metal ion chelation)
Water-Soluble:
Easy to prepare in aqueous solutions for lab use.
Demerits (Disadvantages) of EDTA
Interference with Some Tests:
Can chelate essential metal ions needed for certain biochemical reactions.
For example, EDTA can interfere with calcium or magnesium assays.
Not Suitable for All Tests:
Cannot be used for coagulation studies because it removes calcium.
Potential for Overuse:
High concentrations can cause hemolysis (destruction of red blood cells).
Limited Antimicrobial Activity:
Does not prevent bacterial growth effectively in stored samples.
Q.19 Write a short note on the composition of blood.
Composition of Blood:
Blood is a specialized bodily fluid that circulates through the heart, arteries, veins, and capillaries, performing vital functions such as transport, protection, and regulation. It is composed of two main components: plasma and formed elements.
Plasma (≈55% of blood volume):
Water (90–92%) – serves as a solvent and medium for transporting substances.
Proteins (7–8%) – mainly albumin (maintains osmotic pressure), globulins (immune functions), and fibrinogen (clotting).
Other substances (1–2%) – electrolytes, nutrients (glucose, amino acids), hormones, gases (O₂, CO₂), and waste products (urea, creatinine).
Formed Elements (≈45% of blood volume):
Red Blood Cells (RBCs / Erythrocytes): Carry oxygen from lungs to tissues and CO₂ from tissues to lungs; contain hemoglobin.
White Blood Cells (WBCs / Leukocytes): Part of the immune system; fight infections and foreign substances.
Platelets (Thrombocytes): Play a crucial role in blood clotting and wound repair.
Summary: Blood is a complex fluid composed of plasma and cellular elements, each performing specific functions essential for maintaining life and homeostasis.
Q.20 Difference between RBC & WBC Pipette.
Comparison between the RBC pipette and the WBC pipette, which are commonly used in hematology for counting red and white blood cells:
Purpose
The RBC pipette: Used to dilute and count Red Blood Cells (RBCs)
Used to dilute and count White Blood Cells (WBCs)
Volume Marked
RBC pipette: Usually calibrated to deliver 0.5 µL of blood
WBC pipette: Usually calibrated to deliver 1 µL of blood
Diluting Fluid
RBC pipette: Typically, Hayem’s solution, Gower’s solution, or normal saline
WBC pipette: Typically, Turk’s solution (which contains acetic acid to lyse RBCs and stain WBCs)
Graduations
RBC pipette: Marks for blood and diluting fluid (e.g., 0.5 for blood, 99.5 for diluent to make a 1:200 dilution)
WBC pipette: Marks for blood and diluting fluid (e.g., 0.1 for blood, 0.9 for diluent to make a 1:10 dilution)
Shape & Tip
RBC pipette: Narrower tip for precise RBC handling
WBC pipette: Slightly wider tip; designed to handle WBC suspension with staining
Dilution Factor
RBC pipette: High dilution (usually 1:200 or 1:100)
WBC pipette: Lower dilution (usually 1:20 or 1:100)
Staining Effect
RBC pipette: Does not stain RBCs
Diluting fluid stains WBC nuclei for counting under the microscope
RBC pipette: Small blood volume, high dilution, no staining.
WBC pipette: Larger blood volume, lower dilution, staining solution to visualize WBCs.
Q.21 Describe the qualities of a good blood film.
A good blood film (or blood smear) is crucial for accurate microscopic examination of blood cells. It is used in diagnosing anemia, malaria, and other hematological disorders. The qualities of a good blood film include:
Thin and Even Layer
The film should have a thin “feathered edge” where cells are spread in a single layer.
Cells should not be stacked or overlapping, especially in the monolayer region.
Appropriate Length and Size
The smear should cover 2/3 to 3/4 of the slide and taper gradually toward the feathered edge.
The smear should not be too short or too thick.
Smooth and Uniform
The surface should be smooth without streaks, holes, or ridges.
Avoid “Swiss cheese” effect or uneven thickness.
Proper Cell Distribution
RBCs should be evenly spaced, allowing individual cells to be clearly visible.
WBCs and platelets should not be crowded or clumped.
Feathered Edge Present
The thin edge allows for single-cell examination, which is crucial for differential counts and parasite detection.
Well-Air-Dried and Fixed
The film should be air-dried quickly to prevent cell distortion.
Fixation with methanol is often done for staining, especially for Romanowsky stains.
Minimal Artifacts
Avoid scratches, dust, or debris, as they can interfere with microscopy.
No water or stain pooling that can obscure cell morphology.
Stain Quality (if stained)
Cells should show clear morphology with visible nuclei, cytoplasm, and granules.
The stain should be uniform without patches of over- or under-staining.
Summary: A good blood film is thin, uniform, properly sized, has a clear feathered edge, evenly distributed cells, minimal artifacts, and preserves cell morphology for accurate microscopic evaluation.
Q.22 Discuss the Hb pipette.
Definition: A hemoglobin pipette is a specialized pipette used for measuring a precise volume of blood for hemoglobin estimation. It is used in the cyanmethemoglobin method or other hemoglobin determination techniques.
Design and Types:
Volumetric Accuracy: Hb pipettes are calibrated to deliver a fixed volume, usually 20 µL, 25 µL, or 50 µL, depending on the method.
Graduation:
Usually single or double-marked pipettes.
Micro pipettes allow very precise measurements.
Material:
Made of borosilicate glass to resist chemical reactions.
Some modern versions are plastic with accurate calibration.
Type Examples:
Drabkin’s Pipette: For use with Drabkin’s solution (commonly used in the cyanmethemoglobin method).
Microhematocrit Pipette: Used in micro methods for small blood volumes.
Uses:
To accurately measure a specific volume of whole blood for hemoglobin estimation.
Ensures reproducibility and accuracy in hemoglobin testing.
Compatible with colorimetric or spectrophotometric assays for hemoglobin.
Working Principle:
The blood sample is drawn into the pipette up to the mark.
It is then expelled into the hemoglobin reagent (like Drabkin’s solution).
Mixing ensures hemoglobin conversion to a stable, colored compound.
The color intensity is then measured spectrophotometrically.
Care and Maintenance:
Clean immediately after use with distilled water to avoid clot formation.
Avoid using harsh chemicals that may scratch or damage the pipette.
Store vertically in a pipette stand to prevent breakage.
Calibrate regularly to maintain measurement accuracy.
Cautions
Precision is critical; even a small error in volume can affect hemoglobin estimation.
Always use the correct pipette type for the method (e.g., 20 µL for micro-method, 50 µL for standard methods).
Handle gently as they are fragile and breakable.
SECTION-D
Note: Long answer type questions. Attempt any two questions out of the three questions. (2x8=16)
Q.23 Describe the development stages of Erythropoiesis in detail.
Q.24 Explain the requirements, Preparation, and procedure for venous blood collection.
Q.25 What are Romanowsky stains? Discuss the Leishman stain in detail.
SAMPLE 4
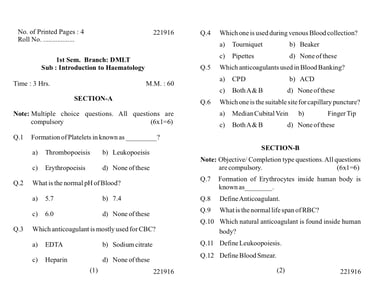
1st Sem. Branch: DMLT Sub: Introduction to Haematology Time : 3 Hrs. M.M.: 60
SECTION-A
Note: Multiple-choice questions. All questions are compulsory (6x1=6)
Q.1 Formation of Platelets in known as _________?
a) Thrombopoiesis b) Leukopoiesis c) Erythropoiesis d) None of these
Q.2 What is the normal pH of Blood?
a) 5.7 b) 7.4 c) 6.0 d) None of these
Q.3 Which anticoagulant is mostly used for CBC?
a) EDTA b) Sodium citrate c) Heparin d) None of these.
Reason: EDTA prevents clotting by chelating calcium and preserves the shape of blood cells, making it ideal for complete blood count (CBC).
Q.4 Which one is used during venous Blood collection?
a) Tourniquet b) Beaker c) Pipettes d) None of these
Reason: A tourniquet is applied to the arm to make the veins more prominent and easier to puncture.
Q.5 Which anticoagulants are used in Blood Banking?
a) CPD b) ACD c) Both A & B d) None of these
Reason: CPD (Citrate-Phosphate-Dextrose) and ACD (Acid-Citrate-Dextrose) are commonly used to preserve blood for transfusion.
Q.6 Which one is the suitable site for capillary puncture?
a) Median Cubital Vein b) Finger Tip c) Both A & B d) None of these
Reason: Capillary blood is usually collected from the fingertip (or heel in infants), not from veins.
SECTION-B
Note: Objective/ Completion type questions. All questions are compulsory. (6x1=6)
Q.7 Formation of Erythrocytes inside the human body is known as________. Ans: Erythropoiesis
Erythropoiesis is the process by which red blood cells (erythrocytes) are formed in the bone marrow of humans. It is stimulated by the hormone erythropoietin, which is primarily produced by the kidneys in response to low oxygen levels in the blood.
Q.8 Define Anticoagulant.
An anticoagulant is a substance that prevents blood from clotting. It can be natural (in the body, for Example, Heparin) or synthetic (added in labs/medical procedures, for example, EDTA, CPD, ACD).
Q.9 What is the normal life span of RBC? Ans: about 120 days
Q.10 Which natural anticoagulant is found inside the human body? Ans Heparin
Q.11 Define Leukoopoiesis.
Leukopoiesis is the process of formation and development of white blood cells (leukocytes) in the bone marrow and lymphoid tissues.
Q.12 Define Blood Smear.
A blood smear is a laboratory technique where a thin layer of blood is spread on a glass slide, stained, and examined under a microscope to study the morphology and count of blood cells.
SECTION-C
Note: Short answer type questions. Attempt any eight questions out of the ten questions. (8x4=32)
Q.13 Write the various functions of blood.
The various functions of blood:
1. Transport Functions: Blood is the main transport medium in the body. It carries:
Oxygen from the lungs to tissues (via red blood cells).
Carbon dioxide from tissues to lungs for exhalation.
Nutrients from the digestive tract to cells (glucose, amino acids, fatty acids, vitamins).
Metabolic wastes (e.g., urea, creatinine) from cells to the kidneys and liver for excretion.
Hormones from endocrine glands to target organs.
2. Regulation Functions: Blood helps maintain homeostasis in the body:
Temperature regulation: Distributes heat from active tissues and helps cool the body.
pH balance: Maintains acid-base balance using buffers (e.g., bicarbonate system).
Fluid balance: Controls water distribution between tissues and blood vessels.
3. Protection Functions: Blood plays a vital role in defending the body:
Clotting: Platelets and clotting factors prevent excessive blood loss after injury.
Immune defense: White blood cells and antibodies fight infections caused by bacteria, viruses, and other pathogens.
Inflammatory response: Blood components help localize infection and promote healing.
4. Transport of Heat: Blood absorbs heat from active tissues and redistributes it, helping maintain core body temperature.
5. Communication: Blood carries chemical messengers like hormones and signaling molecules, enabling communication between organs and systems.
Summary Table for Easy Recall:
Transport: O₂, CO₂, nutrients, hormones, wastes
Regulation: Temperature, pH, fluid balance
Protection: Immunity, clotting, inflammation
Communication: Hormones and chemical signals
Heat Distribution: Maintains body temperature
Q.14 Draw and write the uses of Hb., RBC, and WBC Pipette.
Q.15 Define Plasma and write its compositions.
Definition:
Plasma is a pale yellow, watery liquid component of blood in which blood cells (red blood cells, white blood cells, and platelets) are suspended. Watery fluid makes up about 55% of total blood volume, and it transports nutrients, hormones, proteins, and waste products throughout the body.
Composition of Plasma:
Plasma is mainly composed of:
Water (≈ 90–92%): Acts as a solvent and helps in the transport of substances.
Proteins (≈ 7–8%)
Albumin (≈ 55–60% of plasma proteins): Maintains osmotic pressure and transports substances.
Globulins (≈ 35–38%): Involved in immunity (antibodies) and transport of lipids.
Fibrinogen (≈ 4–5%): Essential for blood clotting.
Regulatory proteins: Hormones and enzymes.
Electrolytes (≈ 0.9%)
Sodium (Na⁺), Potassium (K⁺), Calcium (Ca²⁺), Magnesium (Mg²⁺), Chloride (Cl⁻), Bicarbonate (HCO₃⁻)
Help maintain pH, osmotic balance, and nerve/muscle function.
Nutrients: Glucose, amino acids, fatty acids, vitamins.
Gases: Oxygen (O₂) and carbon dioxide (CO₂) dissolved in plasma.
Waste Products: Urea, creatinine, bilirubin, and other metabolic waste.
Q.16 Describe Non-Calcium chelators as anticoagulants.
Non-calcium chelators are a class of anticoagulants that prevent blood clotting by binding or chelating calcium ions (Ca²⁺) in blood. Calcium is essential for several steps in the coagulation cascade. Without it, the clotting process is inhibited. These agents remove calcium from plasma, thus preventing coagulation.
1. Examples of Non-Calcium Chelators
EDTA (Ethylenediaminetetraacetic acid)
Citrate (Sodium citrate or Trisodium citrate)
Oxalate (Potassium oxalate or Sodium oxalate)
Fluoride + oxalate (for glucose estimation with anticoagulant properties)
2. Mechanism of Action
These agents have a strong affinity for calcium ions. They form stable, soluble complexes with Ca²⁺.
By removing free calcium from the blood, they block activation of clotting factors (e.g., Factor II, VII, IX, X), and prevent the coagulation cascade.
3. Properties & Uses
EDTA
Hematology (CBC, blood smear)
Lavender/purple-top tubes
Preserves cellular morphology; not for coagulation tests
Sodium citrate
Coagulation studies (PT, aPTT)
Blue-top tubes; 9:1 blood:anticoagulant
Reversible by adding calcium in vitro; ideal for clotting tests
Potassium oxalate
Glucose estimation
Gray-top tubes (with fluoride)
Can cause hemolysis if high concentrations are used
Fluoride + oxalate
Blood glucose
Gray-top tubes
Fluoride inhibits glycolysis; oxalate chelates Ca²⁺
4. Advantages
Effective at preventing clotting without altering pH significantly (except oxalate in high concentrations).
EDTA preserves cell morphology for hematology.
Citrate allows reversible anticoagulation (calcium can be added back for assays).
5. Limitations
Cannot be used for calcium measurement in blood (because Ca²⁺ is chelated).
EDTA may interfere with certain enzyme assays.
Oxalate may cause erythrocyte shrinkage or hemolysis in delicate samples.
Summary: Non-calcium chelators act by binding free calcium, which is crucial for coagulation. They are widely used in laboratory medicine, with the choice of agent depending on the type of test (hematology, coagulation, glucose estimation).
Q17 Describe the selection and preparation of the venipuncture site.
1. Selection of the Venipuncture Site
Choosing the correct site is crucial to ensure patient safety, comfort, and successful blood collection. The main factors to consider are visibility, accessibility, and patient condition.
a. Common Sites
Median Cubital Vein
Most preferred site.
Located in the antecubital fossa (inner elbow).
Large, well-anchored, and easily palpable.
Less painful and lower risk of complications.
Cephalic Vein
Lateral side of the antecubital fossa.
Useful if the median cubital vein is not accessible.
Slightly more difficult to palpate in some patients.
Basilic Vein
Medial side of the antecubital fossa.
Last choice due to proximity to nerves and arteries.
Dorsal Hand Veins
Used if antecubital veins are unsuitable.
Smaller, more fragile, and may require smaller needles.
b. Criteria for Selecting a Vein
Vein should be palpable and elastic.
Vein should fill with blood easily.
Avoid veins that are:
Hard, sclerosed, or thrombosed.
Bruised or edematous.
Near areas of infection or injury.
In an arm with IV lines, fistulas, or recent surgery (e.g., mastectomy).
2. Preparation of the Venipuncture Site
Proper preparation prevents infection and ensures patient comfort.
a. Patient Preparation
Explain the procedure to reduce anxiety.
Ensure the patient is seated or lying comfortably.
Position the arm extended and supported with the palm up.
b. Vein Selection and Tourniquet Application
Apply a tourniquet 3–4 inches above the puncture site.
Ask the patient to make a fist without pumping the hand repeatedly.
Palpate the vein to check size, direction, and firmness.
Remove the tourniquet if not suitable, and select another vein if needed.
c. Skin Preparation
Clean the site with an antiseptic (commonly 70% isopropyl alcohol).
Use a circular motion, moving from the center outward.
Allow the skin to air-dry completely (do not blow or wipe).
Avoid touching the site after cleaning.
d. Final Considerations
Check for any sensitive areas or scars.
Ensure all equipment is ready before puncture.
Summary:
Select vein: median cubital > cephalic > basilic > dorsal hand veins.
Assess vein: palpable, elastic, safe location.
Prepare site: explain procedure, apply tourniquet, clean with antiseptic, allow drying.
Q.18 Write the materials & equipment required for capillary puncture.
Materials
Lancet – Single-use sterile lancet (for fingertip or heel puncture).
Alcohol swab – 70% isopropyl alcohol for disinfecting the puncture site.
Gauze or cotton ball – To apply pressure after the puncture.
Gloves – Disposable, sterile gloves for hygiene and safety.
Bandage – Small adhesive bandage to cover the puncture site if needed.
Collection tubes – Microtubes or capillary tubes for collecting blood (EDTA, heparin, or plain, depending on the test).
Capillary tube sealant – Clay or plastic caps for sealing capillary tubes.
Antiseptic wipes – Optional, for extra cleaning if required.
Equipment
Microhematocrit tubes – For hematocrit measurement.
Microcentrifuge – If hematocrit or plasma separation is needed.
Hemoglobinometer or portable hemoglobin device – For quick hemoglobin testing.
Timer or stopwatch – To monitor clotting or test times if necessary.
Sharps container – For safe disposal of used lancets.
Tray or small table – To organize and hold all materials during the procedure.
Q.19 Describe the Vacutainer system in brief.
The Vacutainer system is a widely used closed blood collection system designed for safe, efficient, and sterile collection of blood samples. Here’s a brief description:
Components:
Vacutainer needle – double-ended, with one end for puncturing the vein and the other end for piercing the blood collection tube.
Vacutainer holder (adapter) – a plastic tube holder that secures the needle and the collection tube.
Vacutainer tubes – vacuum-sealed tubes containing specific additives or anticoagulants depending on the test.
Working Principle: The pre-vacuum in the tube automatically draws a precise volume of blood when the needle is inserted into the vein and the tube is attached. This eliminates the need for manual suction or syringes.
Advantages:
Reduces risk of needle-stick injuries and blood exposure.
Maintains sterility and prevents sample contamination.
Allows collection of multiple tubes from a single venipuncture.
Convenient and quick, especially in clinical laboratories.
In short, the Vacutainer system is a safe, closed, and efficient method for blood collection.
Q.20 Write the procedure for the preparation of a Thick blood film.
Q.21 Describe Romanowsky stain in brief.
Romanowsky stain is a type of differential stain used in hematology and cytology. It helps to visualize blood cells, bone marrow cells, and certain parasites (like Plasmodium in malaria).
Composition: It is a mixture of eosin (acid dye) and methylene blue or its derivatives (basic dyes). Common examples include Giemsa, Wright, and Leishman stains.
Principle: The stain differentiates cellular components based on their chemical affinity:
Acidic structures (e.g., cytoplasm) take up eosin → pink/red.
Basic structures (e.g., nuclei, chromatin) take up methylene blue → blue/purple.
Uses:
Identification and morphology of red blood cells, white blood cells, and platelets.
Detection of blood parasites.
Examination of bone marrow aspirates.
In short, Romanowsky stain provides a clear contrast between different cell types, making it essential in hematological diagnostics.
Q.22 Describe Thrombopoiesis in brief.
Thrombopoiesis is the process of platelet (thrombocyte) production in the body.
Site: It occurs mainly in the bone marrow.
Precursor Cells: Platelets are derived from megakaryocytes, large bone marrow cells.
Regulation: The hormone thrombopoietin (TPO), primarily produced by the liver and kidneys, regulates platelet production.
Process:
Hematopoietic stem cells → megakaryocyte progenitors → megakaryocytes.
Megakaryocytes undergo endomitosis (nuclear division without cytoplasmic division) to increase size and ploidy.
Platelets are formed as cytoplasmic fragments of mature megakaryocytes and released into the bloodstream.
Lifespan of Platelets: Approximately 7–10 days in circulation.
Summary: Thrombopoiesis is a TPO-regulated process in the bone marrow where megakaryocytes produce platelets, which play a crucial role in blood clotting.
SECTION-D
Note: Long answer type questions. Attempt any two questions out of the three questions. (2x8=16)
Q.23 Describe the developmental stages of erythrocytes in detail.
Q.24 Explain various anticoagulant vials/tubes with their color code and uses.
Q.25 Explain the requirements, Preparation, and procedure for capillary blood collection.
Dr Pramila Singh
SAMPLE 5
1st Sem / DMLT, Subject: Introduction of Haematology Time : 3 Hrs. M.M.: 60 221916
SECTION-A
Note: Multiple-choice questions. All questions are compulsory (6x1=6)
Q.1 Glacial acetic acid as a diluting fluid is used for counting of:
a) WBC b) RBC c) Platelets d) All of these
Answer: a) WBC. Explanation: Glacial acetic acid lyses RBCs but leaves WBCs intact, making it useful for WBC counting.
Q.2 The cells counted by the Neubauer counting chamber are:
a) RBC b) WBC c) Platelets d) All
Ans: d) All of these. Explanation: The Neubauer chamber can be used to count RBCs, WBCs, and platelets, depending on the diluting fluid used.
Q.3 Blood is mixed with_______ for calculation of HP in sahil’s method
a) Drabkin’s reagent b) N/10 HCI c) Sodium d) none of these
Answer: a) Drabkin’s reagent. Explanation: Drabkin’s reagent converts hemoglobin into cyanmethemoglobin for spectrophotometric measurement.
Q.4 Normal range of WBC in blood is__________
a) 7000-11000/cumm b) 100000-200000/cumm c) 1000-3000 / cumm d) None of these
Answer: a) 7000–11000/cumm. Explanation: Normal adult WBC count is approximately 7,000 to 11,000 per cubic millimeter of blood.
Q.5 DLC stands for_________
a) direct leukocyte count b) differential leukocyte count
c) direct liquid count d) direct leukocyte concentrate
Answer: b) Differential leukocyte count. Explanation: DLC refers to the percentage of different types of WBCs in a blood smear.
Q.6 The WBC pipette has graduations up to mark_____
a) 10 b) 102 c) 101 d) 11
Answer: c) 101, Explanation: WBC counting pipette (Turk’s pipette) is usually graduated up to 101 units for proper dilution of blood for counting.
SECTION-B
Note: Objective/ Completion type questions. All questions are compulsory. (6x1=6)
Q.7 In case of WBC counting, the ratio of blood: diluting fluid is_______
Answer: 1:20 (commonly, 0.1 mL of blood is mixed with 1 mL of WBC diluting fluid).
Q.8 Expand TLC
Total Leukocyte Count
Q.9 Neutrophil nuclei have_______ lobes.
2–5 lobes (typically 3–5 lobes in a mature neutrophil)
Q.10 RBC count _______ in anaemia.
Decreases
Q.11 Full form of PBF is________.
Peripheral Blood Film
Q.12 Leishman stain is a _______ stain.
Answer: Romanowsky-type stain (used for staining blood smears)
SECTION-C
Note: Short-answer type questions. Attempt any eight questions out of the ten questions. (8x4=32)
Q.13 Give the mode of action of the EDTA anticoagulant.
EDTA (Ethylenediaminetetraacetic acid) is a widely used anticoagulant in clinical laboratories. Its mode of action is as follows:
Mode of Action of EDTA:
EDTA is a chelator of divalent and trivalent metal ions, mainly calcium (Ca²⁺).
Calcium ions are essential in the blood coagulation cascade. It helps convert inactive clotting factors to active ones.
EDTS binds to calcium ions, preventing the activation of clotting factors.
As a result, the coagulation cascade is inhibited, and the blood remains in a fluid state suitable for hematological analysis.
Main points for EDTA use:
Usually used in lavender-top (purple) tubes for complete blood counts (CBC) and other hematology tests.
It preserves the morphology of blood cells well, making it ideal for microscopic examination.
Q.14 Explain the structure and uses of the RBC and WBC pipette.
1. RBC (Red Blood Cell) Pipette
Structure:
Type: Graduated capillary pipette.
Material: Usually made of glass.
Capacity: Measures up to 101–102 units on the RBC scale (exact units depend on manufacturer; generally 0–101 divisions for dilution purposes).
Markings: Has two marks:
0.5 mark – for mixing blood with diluting fluid.
101 mark – for completing dilution to 1:200 ratio.
Tip: Narrow tip to draw precise small volumes of blood.
Bulb: For suction or to control fluid.
Uses:
Used to count red blood cells (RBCs) in a hemocytometer.
Measures a precise volume of whole blood.
Helps in preparing a diluted blood sample with Hayem’s or WBC diluting fluid for counting RBCs.
2. WBC (White Blood Cell) Pipette
Structure:
Type: Graduated capillary pipette.
Material: Glass.
Capacity: Measures up to 11 units.
Markings:
0.5 mark – for initial blood collection.
11 mark – to fill to final dilution (usually 1:20 or 1:100 depending on the diluting fluid).
Tip: Narrow, fine tip for accurate blood collection.
Bulb: For suction.
Uses:
Used to count white blood cells (WBCs) in a hemocytometer.
Allows preparation of a diluted sample of blood using Turk’s solution or WBC diluting fluid.
Ensures accurate counting by controlling the dilution ratio.
Summary Table:
Purpose
RBC Pipette: Count red blood cells
WBC Pipette: Count white blood cells
Capacity
RBC Pipette: 0–101 units
WBC Pipette: 0–11 units
Diluting Fluid
RBC Pipette: Hayem’s, Gower’s, or saline
WBC Pipette: Turk’s solution
Tip
RBC Pipette: Narrow
WBC Pipette: Narrow
Dilution Ratio
RBC Pipette: Usually 1:200
WBC Pipette: Usually 1:20 or 1:100
Q.15 Write about the various glassware used in a haematology laboratory?
In a haematology laboratory, proper glassware is crucial for accurate blood analysis, sample handling, and chemical reactions. Different types of glassware are used:
1. Test Tubes
Purpose: Collecting, storing, and centrifuging blood samples.
Types:
Plain glass tubes – for general sample collection.
Anticoagulant-coated tubes – contain EDTA, citrate, or heparin for preventing clotting.
Special Features: Often color-coded caps for easy identification.
2. Beakers
Purpose: Holding, mixing, or heating solutions.
Characteristics: Wide mouth, flat bottom, graduated markings for approximate volume.
Use in Haematology: Preparing reagents like hemolysing solutions or diluents.
3. Conical (Erlenmeyer) Flasks
Purpose: Mixing solutions without spilling, heating liquids.
Characteristics: Narrow neck, wide base.
Use in Haematology: Preparing buffer solutions, diluting blood samples.
4. Volumetric Flasks
Purpose: Preparing solutions of accurate, known concentrations.
Characteristics: Narrow neck with a single graduation mark.
Use in Haematology: Standardizing reagents such as saline or staining solutions.
5. Pipettes
Purpose: Measuring and transferring precise volumes of liquids.
Types:
Volumetric pipettes – deliver a single, precise volume.
Graduated pipettes (Mohr or Serological) – deliver variable volumes.
Pasteur pipettes – for small, approximate transfers.
Use in Haematology: Diluting blood, transferring reagents for tests like CBC or hemoglobin estimation.
6. Burettes
Purpose: Delivering precise volumes, especially in titrations.
Use in Haematology: Rarely used directly; more in reagent preparation.
7. Watch Glasses
Purpose: Holding small samples, evaporating liquids, or covering beakers.
Use in Haematology: Temporary placement of small blood samples or powders.
8. Slides and Cover Slips
Purpose: Observing blood smears under a microscope.
Use in Haematology: Essential for differential WBC counts, morphology studies, and staining procedures.
9. Reagent Bottles
Purpose: Storing chemical reagents safely.
Characteristics: Often amber-colored to protect light-sensitive reagents.
10. Centrifuge Tubes (Glass or Plastic)
Purpose: Spinning blood samples to separate plasma, serum, or cells.
Characteristics: Conical bottom, compatible with centrifuge rotor.
11. Graduated Cylinders
Purpose: Measuring liquid volumes accurately.
Use in Haematology: Preparing reagents and diluents.
Q.16 Write a note on the working of vacutainers.
Vacutainers: Working Principle and Mechanism
Definition:
A vacutainer is a closed blood collection system that allows the safe collection of blood directly into a tube containing anticoagulants or clot activators without exposing the blood to the environment. It is widely used in clinical laboratories for hematology, biochemistry, and serology tests.
Components of a Vacutainer
Vacutainer needle: Double-ended needle; one end penetrates the vein, the other punctures the tube stopper.
Vacutainer tube: Pre-evacuated tube with a specific vacuum, containing either:
Anticoagulants (e.g., EDTA, sodium citrate, heparin)
Clot activators (for serum collection)
Gel separators (for plasma/serum separation)
Plastic holder (or barrel): Holds the tube and needle securely during collection.
Working Mechanism
Vacuum principle:
Each vacutainer tube is pre-evacuated (contains negative pressure) so that when the tube is inserted into the holder and the needle punctures the stopper, the vacuum draws blood automatically into the tube.
The vacuum ensures the exact required volume of blood is collected, preventing overfilling or underfilling.
Closed system safety:
Blood flows directly into the tube without exposure to the environment.
Reduces the risk of contamination and accidental needle-stick injuries.
Mixing with additives:
After collection, tubes containing anticoagulants are gently inverted several times to ensure proper mixing of blood with the additive.
This prevents clotting (in anticoagulant tubes) or ensures clot activation (in serum tubes).
Steps in Blood Collection Using Vacutainer
Select the appropriate tube based on test requirement.
Assemble the needle, holder, and tube.
Clean the venipuncture site and insert the needle into the vein.
Insert the vacutainer tube into the holder; the blood will flow automatically into the tube.
Remove the tube once filled; gently invert if needed.
Withdraw the needle and dispose of it safely.
Advantages of Vacutainers
Accurate volume collection due to the vacuum.
Closed system reduces contamination and infection risk.
Multiple tubes can be collected sequentially using a single puncture.
Compatible with various lab tests due to pre-added additives.
Q.17 Describe the method for the collection of capillary blood?
Method for Collection of Capillary Blood
1. Prepare the Materials
Sterile lancet or capillary puncture device
Alcohol swabs
Sterile gauze
Capillary tubes or microcollection tubes
Gloves
Labels for specimen
2. Patient Preparation
Explain the procedure to the patient.
Wash your hands and put on gloves.
Ensure the patient’s hand is warm to increase blood flow (cold fingers can reduce flow).
3. Site Selection
Common sites:
Finger: middle or ring finger of non-dominant hand
Heel: in infants under 1 year old
Clean the site with an alcohol swab and allow it to air dry.
4. Puncture
Use a sterile lancet or puncture device to make a quick, shallow puncture.
For finger puncture: puncture perpendicular to the fingerprint lines, usually on the lateral side of the fingertip.
Avoid puncturing the tip or central pad.
5. First Drop Removal
Wipe away the first drop of blood with sterile gauze to prevent tissue fluid contamination.
6. Collect the Blood
Gently massage or apply light pressure to the finger toward the puncture site to encourage blood flow.
Collect blood into a capillary tube or microcollection tube without squeezing too hard.
Fill the required volume for the test.
7. Post-collection Care
Apply sterile gauze and pressure to stop bleeding.
Bandage the puncture site if necessary.
Dispose of the lancet safely in a sharps container.
8. Label and Transport
Label the collected sample immediately.
Transport to the laboratory according to test requirements.
Points to Remember
Do not squeeze excessively; it can dilute blood with tissue fluid.
Always use a new sterile lancet for each patient.
Maintain proper hygiene and safety to prevent infection.
Q.18 Write the different stages of thrombopoiesis.
Stages of Thrombopoiesis
Hematopoietic Stem Cell (HSC) Stage
Multipotent stem cells in the bone marrow that can differentiate into all blood cell types.
HSC → Common Myeloid Progenitor (CMP).
Megakaryocyte Progenitor Stage
CMP differentiates into Megakaryocyte Colony-Forming Unit (CFU-Meg).
These are committed progenitor cells that will only produce megakaryocytes.
Megakaryoblast Stage
The first recognizable stage of the megakaryocyte lineage.
Large cell with a high nuclear-to-cytoplasmic ratio.
Undergoes endomitosis (nuclear replication without cell division), leading to polyploidy.
Promegakaryocyte Stage
Intermediate stage between megakaryoblast and mature megakaryocyte.
Nucleus becomes lobulated; cytoplasm begins to develop granules.
Cell size increases significantly.
Mature Megakaryocyte Stage
Large, polyploid cell with abundant cytoplasm containing alpha and dense granules.
The cytoplasm extends into proplatelets, which are long cytoplasmic processes.
Platelet Formation (Thrombocyte Stage)
Proplatelets fragment into thousands of platelets that enter the bloodstream.
Platelets are small, anucleate cell fragments essential for hemostasis.
Regulation:
Thrombopoietin (TPO), mainly produced by the liver, is the primary hormone regulating thrombopoiesis.
Other cytokines like IL-3, IL-6, and IL-11 also support megakaryocyte development.
Q.19 Define blood and give its function.
Definition of Blood: Blood is a specialized bodily fluid that circulates throughout the body via the heart, arteries, veins, and capillaries. It is composed of plasma (the liquid part) and formed elements (red blood cells, white blood cells, and platelets).
Functions of Blood:
Transport:
Carries oxygen from the lungs to body tissues and carbon dioxide from tissues to the lungs.
Transports nutrients from the digestive system to cells.
Removes waste products for excretion (e.g., urea, creatinine).
Transports hormones from endocrine glands to target organs.
Regulation:
Maintains body temperature by distributing heat.
Regulates pH and fluid balance.
Protection:
White blood cells defend against infections and foreign substances.
Platelets help in blood clotting to prevent excessive bleeding.
Plasma contains antibodies and clotting factors for immunity and coagulation.
Other Functions:
Acts as a medium for the exchange of gases, nutrients, and wastes.
Helps maintain homeostasis in the body.
Q.20 Enlist the various equipment used for venous blood collection.
List of equipment commonly used for venous blood collection in a clinical or laboratory setting:
1. Blood Collection Needles
Hypodermic needles (various gauges, e.g., 21G, 23G)
Butterfly needles (winged infusion sets) – for difficult veins or pediatric patients
2. Collection Systems
Vacutainer system (closed system with vacuum tubes)
Syringes (for manual blood collection)
3. Blood Collection Tubes
Vacutainer tubes with specific additives:
EDTA (anticoagulant) – for hematology
Citrate – for coagulation tests
Heparin – for chemistry tests
Serum separator tubes (SST) – for serum tests
4. Accessories
Tourniquet – to constrict the vein
Alcohol swabs or antiseptic wipes – for site cleaning
Cotton balls or gauze – to apply pressure after collection
Adhesive bandages – to cover the puncture site
5. Safety Equipment
Gloves – for infection control
Sharps container – for safe disposal of needles
Protective gowns or aprons (optional, depending on setting)
6. Miscellaneous
Labels – to properly mark the collected samples
Tray or holder – to organize equipment during collection
Q.21 Write a short note on leukopoiesis.
Leukopoiesis
Leukopoiesis is the process of formation and development of white blood cells (leukocytes) from hematopoietic stem cells in the bone marrow. White blood cells are crucial for the body’s defense mechanisms against infections, foreign substances, and abnormal cells.
Main Points:
Origin: All leukocytes arise from multipotent hematopoietic stem cells (HSCs) in the bone marrow.
Lineages:
Myeloid lineage → gives rise to granulocytes (neutrophils, eosinophils, basophils) and monocytes.
Lymphoid lineage → gives rise to lymphocytes (B cells, T cells, and NK cells).
Regulation: Controlled by growth factors and cytokines such as colony-stimulating factors (CSFs) and interleukins (ILs).
Stages: Stem cells → progenitor cells → precursor cells (myeloblasts, lymphoblasts, etc.) → mature leukocytes.
Clinical relevance: Disorders in leukopoiesis can lead to leukopenia (low WBC count), leukocytosis (high WBC count), or leukemia (malignant proliferation of WBCs).
Summary: Leukopoiesis is a vital process for maintaining the immune system, ensuring a steady supply of functional white blood cells to protect the body.
Q.22 Write down about the properties of a good blood film.
Properties of a Good Blood Film
Even Thickness (Gradient)
The film should be thick at the start (proximal end) and gradually thinner towards the feathered edge.
The thick area is for examining red blood cells (RBCs); the thin “feathered edge” is for examining white blood cells (WBCs) and platelets.
Feathered Edge
The end of the smear tapers into a fine, almost transparent edge.
Provides a single layer of cells without overlapping—essential for accurate WBC and platelet counts and morphology assessment.
Uniform Cell Distribution
RBCs should be evenly spread without clumping or gaps.
Avoid piling up of cells (rouleaux formation) or areas with too few cells.
Proper Size and Length
It should be long enough for examination, typically 2–3 cm long.
Not too short (insufficient cells) or too long (difficult to stain evenly).
No Streaks or Holes
Smooth smear without thick streaks, holes, or ridges.
Ensures uniform staining and clear visualization.
Correct Cell Morphology
RBCs, WBCs, and platelets should retain natural shapes.
Avoid distortion caused by excessive pressure when spreading.
Clean Background
No dust, oil, or debris that may interfere with microscopic observation.
Proper Staining Capability
Film should allow even uptake of stains like Wright or Giemsa for accurate identification.
Tip: The ideal blood film is thin enough to see individual cells at the feathered edge but thick enough at the body of the smear for overall RBC morphology. Always prepare smears immediately after blood collection for best results.
SECTION-D
Note: Long answer type questions. Attempt any two questions out of the three questions. (2x8=16)
Q.23 Explain the principle and types of Romanowsky stain. Explain anyone in detail.
Q.24 Write a note on the blood cell counter.
Q.25 Write a note on different types of anticoagulants. Explain any two with their merits and demerits.
Dr Pramila Singh
SAMPLE 5 1st Sem. / DMLT. Subject: Introduction to Haematology Time: 3 Hrs. M.M.: 60
SECTION-A
Note: Multiple-choice questions. All questions are compulsory (6x1=6)
Q.1 The Function of erythrocytes includes
a) Acid-base balance b) Maintains the viscosity of blood c) Ion balance d) All
Answer: d) All Explanation: Erythrocytes (RBCs) are primarily responsible for oxygen transport, but they also contribute to acid-base balance, blood viscosity, and ion balance.
Q.2 Plasma without fibrinogen is termed as
a) Hemoglobin b) Hemolysed RBCs c) Red blood cells d) Serum
Answer: d) Serum Explanation: When plasma clots, fibrinogen is converted to fibrin, and the remaining liquid is called serum.
Q.3 Counting chamber used for counting blood cells
a) Neubauer chamber b) Burker chamber c) Fuchs-Rosenthal chamber d) All
Answer: a) Neubauer chamber. Explanation: The Neubauer chamber is the standard hemocytometer used for counting blood cells. Burker and Fuchs-Rosenthal are variations, but Neubauer is the most common.
Q.4 The Site of venipuncture for the collection of the sample is located at
a) Median cubital vein b) Arm with intravenous line c) Veins on back of hand and neck d) All.
Answer: a) Median cubital vein. Explanation: The median cubital vein in the antecubital fossa is the preferred site for blood collection due to ease of access and safety. Other veins are used only if necessary.
Q.5 Upon treating with Romanowsky stains, red cells are stained
a) Orange color b) Black color c) Pink color d) Blue color
Answer: c) Pink color. Explanation: Romanowsky stains (like Giemsa or Wright) stain RBCs pink, while nuclei of WBCs stain blue to purple.
Q.6 During erythropoiesis, which of the cells are formed first
a) Pronormoblast b) Early normoblast c) Reticulocyte d) Late normoblast
Answer: a) Pronormoblast. Explanation: The sequence in erythropoiesis:
Pronormoblast → Early normoblast → Late normoblast → Reticulocyte → Mature RBC
SECTION-B
Note: Objective/ Completion type questions. All questions are compulsory. (6x1=6)
Q.7 Tell the sites of poiesis for children and adults
1. Children: Mainly in the bone marrow of all bones, especially long bones like the femur and tibia.
2. Adults: Primarily in the axial skeleton, including vertebrae, sternum, ribs, skull, and pelvis.
Q.8 Give the full form of EDTA
Ethylenediaminetetraacetic Acid
Q.9 Identify the additive present in the colored vacutainer
Sodium citrate (used for coagulation studies)
Q.10 Name the organ secreting erythropoietin
1. Kidneys (mainly)
2. Liver (minor contribution during fetal life)
Q.11 Define the term phlebotomy
Phlebotomy is the process of making an incision in a vein to collect blood for diagnostic or therapeutic purposes.
Q.12 Name the test performed for blood screening procedures
Examples include:
Complete Blood Count (CBC)
Blood grouping and crossmatching
Infectious disease screening: HIV, Hepatitis B & C, Syphilis
Coagulation tests (if required)
SECTION-C
Note: Short answer type questions. Attempt any eight questions out of ten questions. (8x4=32)
Q.13 Discuss any four anticoagulants, stating their principle of action and therapeutic indications
Four commonly used anticoagulants in medical laboratories, including their principle of action and therapeutic indications:
1. EDTA (Ethylenediaminetetraacetic acid)
Chelates calcium ions (Ca²⁺), which are essential for the coagulation cascade, thereby preventing clot formation.
- Hematology tests (CBC, blood smear, ESR)- Preserves cell morphology for microscopic examination- DNA/RNA studies
2. Sodium Citrate
Binds calcium reversibly by forming calcium-citrate complexes; allows for plasma separation without affecting clotting factors.
- Coagulation studies (PT, aPTT)- Blood transfusion studies- Platelet function tests
3. Heparin
Activates antithrombin III, which inactivates thrombin and factor Xa, inhibiting fibrin formation.
- Clinical chemistry tests requiring plasma (e.g., electrolyte analysis)- Blood gas analysis- Some cytogenetic studies
4. Oxalates (e.g., potassium oxalate)
Combines with calcium to form insoluble calcium oxalate, preventing clotting.
- Glucose estimation (commonly used with fluoride)- Some enzymatic assays- Occasionally used in hematology, but less common than EDTA
Key Notes:
EDTA is preferred for hematology because it preserves cellular components well.
Sodium citrate is used in coagulation studies because it can be reversed by adding calcium during testing.
Heparin is not ideal for hematology as it may distort cell morphology, but it is excellent for chemistry tests.
Oxalates are mainly used when glucose preservation is required, as they inhibit glycolysis.
Q.14 Describe the methods for the estimation of hemoglobin.
1. Sahli’s Method (Acid Hematin Method)
Principle:
Hemoglobin is converted into acid hematin by treating it with dilute hydrochloric acid. The brown color formed is compared with a standard comparator, and the hemoglobin concentration is estimated.
Procedure:
Take Sahli’s hemoglobin tube (graduated).
Add 0.1 N HCl up to the lowest mark of the tube.
Using a Sahli’s pipette (20 µL), draw blood up to the mark.
Wipe the outside of the pipette and transfer the blood into the acid in the tube.
Mix thoroughly and allow it to stand for about 10 minutes (to ensure complete conversion of Hb into acid hematin).
Then dilute the mixture with distilled water, drop by drop, while stirring with a glass rod, until the color matches with the standard brown-colored glass in the comparator.
Read the hemoglobin concentration directly from the graduated scale in g/dL.
Limitations:
Visual color matching → subjective error.
Not highly accurate.
Turbidity in blood (lipemia, high WBC) can interfere.
2. Cyanmethemoglobin Method (Drabkin’s Method)
Principle:
Blood is treated with Drabkin’s reagent (containing potassium cyanide + potassium ferricyanide + dihydrogen potassium phosphate).
Hemoglobin is converted into cyanmethemoglobin, a stable colored compound.
The intensity of the color is measured spectrophotometrically at 540 nm, which is proportional to the hemoglobin concentration.
Procedure:
Take 5 mL of Drabkin’s reagent in a test tube or cuvette.
Add 20 µL of blood using a micropipette.
Mix gently and allow to stand for 5–10 minutes for full conversion.
Measure absorbance at 540 nm against a reagent blank using a colorimeter/spectrophotometer.
Compare the absorbance with that of a standard cyanmethemoglobin solution.
Calculate the hemoglobin concentration in g/dL.
Advantages:
Highly accurate and reliable.
Internationally recommended by ICSH (International Committee for Standardization in Hematology).
Measures all forms of Hb except sulfhemoglobin.
Summary Table for Students
Principle
Sahli’s Method (Acid Hematin)Hb + HCl → Acid Hematin
Cyanmethemoglobin (Drabkin’s) Method: Hb + Drabkin’s reagent → Cyanmethemoglobin
Measurement
Sahli’s Method (Acid Hematin): Visual color matching
Cyanmethemoglobin (Drabkin’s) Method: Spectrophotometer at 540 nm
Accuracy
Sahli’s Method (Acid Hematin): Less accurate, subjective
Cyanmethemoglobin (Drabkin’s) Method: Highly accurate, standard method
Time
~10–15 min
Cyanmethemoglobin (Drabkin’s) Method: ~5–10 min
Standardization
Not standardized internationally
Cyanmethemoglobin (Drabkin’s) Method: ICSH-recommended
Q.15 Why is the determination of red cell indices considered clinically significant?
The determination of red cell indices (MCV, MCH, and MCHC) is considered clinically significant. They provide valuable information about the size and hemoglobin content of red blood cells. This helps in the diagnosis and classification of different types of anemia and related disorders.
Clinical Significance of Red Cell Indices:
Mean Corpuscular Volume (MCV):
Indicates the average size of red blood cells.
Helps classify anemia as:
Microcytic (small cells, e.g., iron deficiency anemia, thalassemia)
Normocytic (normal size, e.g., acute blood loss, hemolytic anemia)
Macrocytic (large cells, e.g., vitamin B12 or folate deficiency).
Mean Corpuscular Hemoglobin (MCH):
Shows the average amount of hemoglobin per red cell.
Reduced MCH suggests hypochromic cells (as in iron deficiency).
Increased MCH is seen in macrocytic anemias.
Mean Corpuscular Hemoglobin Concentration (MCHC):
Reflects the concentration of hemoglobin in a given volume of red cells.
Low MCHC = hypochromia (iron deficiency anemia).
Normal MCHC = normochromia (e.g., acute blood loss anemia).
High MCHC = rare (hereditary spherocytosis, severe dehydration).
Helps Differentiate Types of Anemia:
For example:
Iron deficiency anemia → Low MCV, low MCH, low MCHC (microcytic hypochromic).
Vitamin B12 / Folate deficiency → High MCV, normal or high MCH (macrocytic).
Thalassemia trait → Low MCV, but normal MCHC, with high RBC count.
Guides Further Investigations and Treatment:
Identifies whether the anemia is due to iron, vitamin deficiency, chronic disease, or genetic disorder.
Helps doctors select appropriate therapy (iron supplementation, vitamin replacement, transfusion, etc.).
In short, Red cell indices are clinically significant because they are essential for the diagnosis, classification, and management of anemia and provide insights into the underlying cause of red blood cell abnormalities.
Q.16 Distinguish between capillary and venous collection of blood samples
Q.17 Describe the method of preparation of an ideal blood film
Method of Preparation of an Ideal Blood Film
Requirements
Clean, grease-free glass slides (2 slides).
Capillary blood (finger prick) or EDTA anticoagulated venous blood.
Sterile lancet, cotton swab.
Procedure
1. Collection of blood
Place a small drop of blood near one end of the slide (about 1–2 mm in diameter).
2. Spreader preparation
Hold another clean slide (the spreader) at an angle of 30–45° to the slide with the blood drop.
3. Spreading the film
Bring the spreader backward to touch the drop of blood.
Allow the drop to spread along the edge of the spreader.
Push the spreader forward smoothly and rapidly in one stroke, producing a thin film.
4. Drying
Air-dry the smear quickly.
Do not blow or heat the slide.
5. Fixation and staining (for examination)
Fix in methanol (if required) and stain with Romanowsky stains (Leishman, Giemsa, or Wright).
Characteristics of an Ideal Blood Film
The smear covers two-thirds to three-fourths of the slide.
Film has a tongue-shaped appearance: thick at the head, thin at the tail.
Even distribution of cells (not clumped).
The feathered edge (tail end) is thin, with cells lying singly and not overlapping.
RBCs appear evenly spaced, without rouleaux formation.
Leukocytes are well preserved and distributed throughout.
In short: An ideal blood film is prepared by placing a small drop of blood on a slide and spreading it smoothly at a 30–45° angle with another slide, followed by air-drying. It should be tongue-shaped, cover 2/3 of the slide, and show evenly distributed, non-overlapping blood cells.
Q.18 How does the capillary and venous collection of blood samples differ?
Comparison between capillary blood collection and venous blood collection:
🔹 Capillary Blood Collection
Source: Taken from capillaries (small blood vessels between arterioles and venules).
Site: Commonly fingertip, heel (infants), or earlobe.
Method: Skin is punctured with a lancet; blood is collected drop by drop.
Volume: Small (microliters to <1 mL).
Pain/Discomfort: Less invasive, less painful.
Uses:
Glucose monitoring
Hemoglobin estimation
Newborn screening
Point-of-care tests (POCT)
Advantages: Quick, easy, no need for veins, minimal risk.
Limitations:
Limited volume
Hemolysis and contamination are more common
It may not be suitable for coagulation or many biochemical tests
🔹 Venous Blood Collection
Source: Drawn from a vein (usually the median cubital vein in the arm).
Site: Antecubital fossa (elbow bend), dorsum of hand, forearm veins.
Method: Vein puncture with a syringe or evacuated tube system.
Volume: Large (several milliliters to >10 mL).
Pain/Discomfort: More invasive, may cause bruising or discomfort.
Uses:
Most routine diagnostic tests (hematology, biochemistry, serology)
Blood culture
Blood transfusion collection
Advantages: Provides sufficient volume, better sample quality, and a wide range of tests possible.
Limitations: Requires trained personnel, risk of hematoma, fainting, or infection.
Key Difference in Simple Terms:
Capillary collection → small amount, quick, used for rapid/simple tests.
Venous collection → large amount, more invasive, used for most laboratory investigations.
Q.19 Tell the different ways of disposal for blood and related products
Disposal of blood and related products (like blood bags, plasma, serum, and contaminated items) must follow strict Biomedical Waste Management guidelines to prevent infection, contamination, and environmental hazards.
the Main ways of disposal:
1. Incineration
Method: Burning of blood-soaked items, blood bags, and sharps in a biomedical incinerator at high temperature (>1200°C).
Use: Suitable for large-scale hospitals and blood banks.
Limitation: Expensive; requires proper air pollution control.
2. Autoclaving / Hydroclaving
Method: Steam sterilization (121–134°C) of contaminated blood products and plastic disposables.
Use: For microbiological decontamination before shredding or recycling.
Limitation: Not suitable for liquid blood in large volumes.
3. Chemical Disinfection
Method: Adding chemical disinfectants (e.g., 1% sodium hypochlorite, 5% phenol, or glutaraldehyde) to liquid blood and small quantities of contaminated products.
Use: For liquid blood and small spills before final disposal.
Limitation: Ineffective for large-scale waste.
4. Deep Burial (in rural/remote areas)
Method: Blood-soaked waste or small volumes of blood are disposed in a deep burial pit (2 meters deep, lined with lime and soil).
Use: Allowed only in remote/rural areas where incineration is not available.
Limitation: Risk of contamination of groundwater if not properly managed.
5. Sewer Disposal (after disinfection)
Method: Liquid blood or plasma is treated with disinfectant (e.g., sodium hypochlorite) and then discharged into the sewer.
Use: For laboratory and small hospital settings.
Limitation: Only permissible after proper disinfection.
6. Plasma Fractionation / Reuse (specialized use)
Method: Surplus plasma from blood banks may be sent for fractionation to extract useful proteins (e.g., albumin, clotting factors).
Use: Scientific recycling before waste disposal.
7. Sharps Disposal (Needles, lancets, syringes with blood residue)
Method: Collected in puncture-proof containers → autoclaving or dry heat sterilization → shredding → incineration or disposal in sharps pits.
Color Coding for Biomedical Waste (as per guidelines):
Yellow bag: Blood bags, blood-soaked materials, body fluids → Incineration/Deep burial.
Red bag: Contaminated tubing, syringes (without needles), IV sets → Autoclaving/shredding/recycling.
White (translucent) container: Sharps → Autoclaving/dry heat sterilization/shredding.
Q.20 List the different types of glassware used in a hematology laboratory.
In a hematology laboratory, different types of glassware are used for the collection, preparation, and analysis of blood samples.
Types of Glassware in Hematology Laboratory
Test Tubes – For collection and holding blood samples, especially for anticoagulated and clotted blood.
Centrifuge Tubes – Used for separating plasma/serum from cells after centrifugation.
Pipettes (Graduated / Volumetric / Pasteur Pipettes) – For accurate measurement and transfer of blood or reagents.
Hemocytometer (Counting Chamber with Cover Glass) – For manual counting of red blood cells (RBCs), white blood cells (WBCs), and platelets.
Slides (Microscope Glass Slides) – For preparing peripheral blood smears.
Cover Slips – To cover blood smears on slides for microscopic examination.
Reagent Bottles (Glass Bottles with Stoppers) – For storing hematology stains, anticoagulant solutions, and reagents.
Beakers – For mixing and holding larger volumes of reagents.
Conical Flasks (Erlenmeyer Flasks) – For preparing and storing staining solutions like Wright’s, Giemsa, or Leishman stain.
Graduated Cylinders – For measuring liquids used in the preparation of reagents.
Though plasticware is replacing glassware in many modern labs (e.g., disposable plastic test tubes, pipette tips, and containers), glass remains important for accuracy, chemical resistance, and preparation of permanent reagents.
Q.21 Infer the hematological investigations and cytochemical reactions in chronic lymphocytic leukemia
hematological investigations and cytochemical reactions in Chronic Lymphocytic Leukemia (CLL):
Hematological Investigations in CLL
Complete Blood Count (CBC):
Leukocytosis – usually >15,000/µL, can rise to >100,000/µL.
Absolute lymphocytosis – mature-appearing small lymphocytes predominate.
Anemia – may occur due to bone marrow infiltration or autoimmune hemolysis.
Thrombocytopenia – due to marrow replacement or immune destruction.
Peripheral Blood Smear:
Numerous small, mature lymphocytes with condensed chromatin and scant cytoplasm.
Smudge (basket) cells – fragile lymphocytes damaged during smear preparation (characteristic).
Bone Marrow Examination:
Hypercellular marrow with >30% lymphocytes.
Diffuse, interstitial, or nodular infiltration of small mature lymphocytes.
Immunophenotyping (Flow Cytometry):
Confirms CLL diagnosis by detecting a monoclonal B-cell population.
Characteristic markers: CD5+, CD19+, CD20(dim), CD23+, weak surface immunoglobulin (sIg).
Differentiates CLL from other lymphoproliferative disorders (e.g., mantle cell lymphoma).
Other Hematological Features:
Positive direct Coombs’ test in autoimmune hemolytic anemia (seen in ~10–25% cases).
Hypogammaglobulinemia – due to defective antibody production → recurrent infections.
Cytochemical Reactions in CLL
Myeloperoxidase (MPO) stain: Negative (rules out myeloid leukemia).
Sudan Black B: Negative (not of myeloid origin).
Periodic Acid-Schiff (PAS): Usually negative or weak diffuse positivity (not specific).
Acid Phosphatase: Negative (helps to differentiate from T-cell prolymphocytic leukemia, which can show positivity).
Non-specific esterase (NSE): Negative (rules out monocytic leukemia).
Summary:
Hematology: Marked lymphocytosis, smudge cells, marrow infiltration, immunophenotyping with CD5+, CD23+.
Cytochemistry: Mostly negative reactions (MPO, SBB, NSE), helping rule out myeloid and monocytic leukemias.
Q.22 List four abnormalities found in RBCs along with the underlying cause.
four common abnormalities in RBCs with their underlying causes:
Sickle Cells
Appearance: Crescent or sickle-shaped RBCs.
Cause: Mutation in the β-globin gene → production of abnormal hemoglobin (HbS) → polymerization under low oxygen tension → distortion of RBC shape.
Seen in: Sickle cell anemia.
Spherocytes
Appearance: Small, round, sphere-shaped RBCs lacking central pallor.
Cause: Defect in RBC membrane proteins (spectrin, ankyrin) leading to loss of membrane surface area.
Seen in: Hereditary spherocytosis, autoimmune hemolytic anemia.
Target Cells (Codocytes)
Appearance: Bull’s-eye-like RBCs with central staining.
Cause: Increased surface membrane-to-volume ratio.
Seen in: Thalassemia, liver disease, post-splenectomy.
Schistocytes (Fragmented RBCs)
Appearance: Irregularly shaped, fragmented RBCs.
Cause: Mechanical damage to RBCs due to passage through fibrin strands or prosthetic heart valves.
Seen in: Microangiopathic hemolytic anemia (DIC, TTP, HUS), mechanical hemolysis.
SECTION-D
Note: Long answer type questions. Attempt any two questions out of three questions. (2x8=16)
Q.23 Classify the Romanowsky stains. Describe the principle and infer the results obtained for different stains
Q.24 Describe the different methods used for the measurement of ESR values. Analyze the significance of such determinations
Q.25 Summarize the various anticoagulants, signifying their color codes, mode of action, uses, relative advantages and disadvantages
Subject: Introduction to Haematology 221916 Time : 3 Hrs. M.M.: 60 1st Year / DMLT.
UNIT I Introduction to Haematology 1.1 Various glassware/plasticware used in Haematology Labs. (Hb. Tube, Hb. Pipette (RBC Pipette, WBC Pipette). 1.2 Introduction to blood. 1.3 Definition & Composition 1.4 Cells-WBC (Granulocytes-Neutrophils, Eosinophils& Basophils), (Agranulocytes Lymphocytes & Monocytes), RBC, Platelets. 1.5 Plasma & its components 1.6 Function-cell functions & plasma functions. 1.7 Formation of blood (Erythropoiesis, Leukopoiesis, and Thrombopoiesis)
Section A
The study of blood and its. components are called a) Haematology, b) Microbiology, c) Histology, d) None of these.
What is the normal life span of RBC? a) 180 days b) 120 days c) 45 days d) None of these
Formation of Platelets in known as _________? a) Thrombopoiesis b) Leukopoiesis c) Erythropoiesis d) None of these
What is the normal pH of Blood? a) 5.7 b) 7.4 c) 6.0 d) None of these
Normal range of WBC in blood is__________ a) 7000-11000/cumm b) 100000-200000/cumm c) 1000-3000 / cumm d) None of these
The function of erythrocytes includes a) Acid-base balance, b) Maintains viscosity of blood, c) Ion balance, d) All
Plasma without fibrinogen is termed as a) Hemoglobin b) Hemolysed RBCs c) Red blood cells d) Serum
During erythropoiesis, which of the cells are formed first? a) Pronormoblast b) Early normoblast c) Reticulocyte d) Late normoblast
Section B
Define Haematology
Blood is a ________tissue
Formation of erythrocytes inside the human body is known as
Formation of WBC inside the human body is known as_______________.
Write the components of blood
Define Thrombopoiesis.
What is the normal life span of RBC
What is capillary blood?
Formation of Leukoeytes inside human body is known as _______
Define Leukoopoiesis
Tell the sites of poiesis for children and adults
Neutrophils nucleus have _______ lobes.
RBC count _______ in anaemia.
Name the organ secreting erythropoietin
Section C
Define blood and write its composition, OR Write a short note on the composition of blood
Define blood and give its function.
Write the various functions of blood.
Write the uses of the RBC and WBC Pipette.
Define Plasma and write its compositions
Write the different stages of thrombopoiesis.
Write a short note on leukopoiesis.
List the different types of glassware used in a hematology laboratory.
Draw and explain any four glassware used in the Haematology Laboratory
Write the difference between Serum & Plasma.
Draw and write the uses of Hb., RBC, and WBC Pipette
Why is the determination of red cell indices considered clinically significant?
List four abnormalities found in RBCs along with the underlying cause
Section D
Describe the developmental stages of erythrocytes in detail
Describe the development stages of Erythropoiesis in detail.
Dr Pramila Singh
