Reproductive System
Reproductive System: Male and female reproductive system, The ovarian cycle and ovulation, Fertilization. MLT IInd Sem HSBTE
Dr Pramila Singh
4/28/202412 min read
Reproductive System: Male and female reproductive system, The ovarian cycle and ovulation, Fertilization. MLT IInd Sem HSBTE
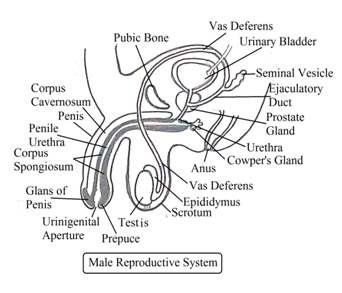
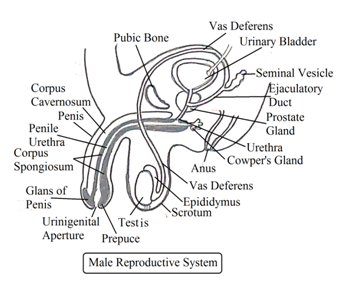
MALE REPRODUCTIVE SYSTEM
Anatomy of the male reproductive system: The male reproductive system consists of internal and external organs. The male reproductive organs are divided into primary sex organs, secondary sex organs, and Accessory glands.
Primary Sex Organs in Male (Gonads): In the male, the primary sex organ is the testis. Secondary sex organs in the male are Scrotum, Epididymis, Vasa deferentia (Vas deferens), Ejaculatory Duct, Urethra, and Penis. Accessory glands are seminal vesicles, prostate glands, and bulbourethral glands.
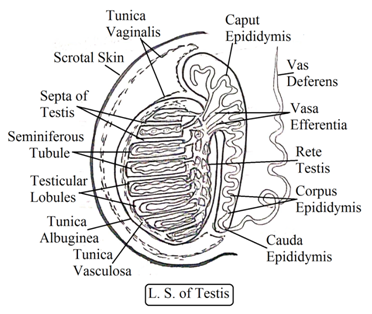
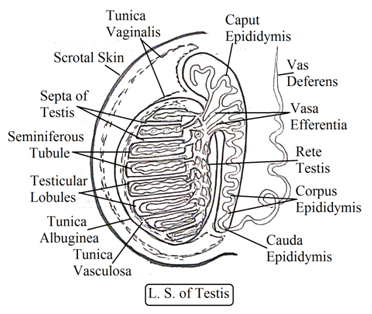
Testes: (Singular: Testis): Testes are the primary sex organ in males. The human male body has two testes inside the scrotum. The spermatic cord holds each testis inside the scrotum. Testes are oval-shaped, soft, pinkish, and smooth structure. It is a tubular gland with three layers of protective covering called tunica (Pl. tunicae).
Tunicae: It is a protective covering. It has three layers. These are Tunica vaginalis, Tunica albujinea and Tunica vasculosa.
Each testis has about 250 testicular lobules. The testicular lobule has highly coiled 70 to 80 cm long seminiferous tubules. Seminiferous tubules join together to form tubuli recti, a straight duct.
Interstitial cells: (Leydig’scells): They are present in between seminiferous tubules. These interstitial cells secrete androgen hormones. This is a male sex hormone, eg. testosterone.
Tubuli Recti forms a network called rete testis.
Seminiferous tubule epithelium has two types of cells: germinating epithelium cells and supporting cells. Germinating epithelium cells (Spermatogenic cells) are also known as spermatogonia. Spermatogonia form spermatids. Spermatids grow and form spermatozoa. The formation of spermatozoa from spermatogenic cells is called spermatogenesis.
Seminiferous tubules also contain some tall Sertoli cells. It is a supporting cell. It provides nutrition to developing sperm. Sertoli cells also provide nutrition to maturing (developing) sperms.
Male Secondary sex organs
Scrotum: The scrotum is a deeply pigmented skin pouch that hangs between both thighs. It is divided into two scrotal sacs by septum scroti. Each scrotal sac contains one testis. Septum scroti can be marked externally as raphe. The scrotum maintains the optimum temperature for the testis. The temperature around the testis is always 2 degrees lower than the body's internal temperature. It is the ideal temperature for spermatogenesis.
Vasa efferentia: It connects the rete testis and epididymis. Vasa efferentia has ciliated epithelium which helps spermatozoa movement.
Epididymis: Union of vasa efferentia forms epididymis in each testis. It is a long, closely coiled narrow compact tubular mass present in the inner side of each testis. There are three parts of the epididymis. Epididymis at upper end of testis is called caput epididymis,. Epididymis at middle of testis is called corpus epididymis. Epididymis at the lower end (of the testis is called cauda epididymis.
Epididymis secretes nutrient fluid that nourishes spermatozoa (sperm). It also stores sperm till its ejaculation.
Vas deferens: (Sperm duct): Cauda epididymis comes out from each scrotal sac called vas deferens. It joins the duct from seminal vesicles and forms the ejaculatory duct. They transport sperm from the testis to the urethra to the outside body during ejaculation.
Ejaculatory duct: The ejaculatory duct enters into the prostate gland and unites with the prostatic urethra to form the urinogenital duct. Sperm combines with whitish secretion from the duct of the seminal vesicle to form semen. The ejaculatory duct carries sperm and seminal vesicle fluids
Urethra: Urethra is a fibromuscular tubular duct that carries urine from the urinary bladder and semen from the ejaculatory duct. It passes through the penis and opens into the outside body. The urethra transports both semen and urine. The male urethra is longer than the female urethra. The male urethra has the following parts: Urinary urethra, Prostatic urethra, Membraneous urethra, and penile urethra.
The urethra has two sphincters: The internal sphincter and the external sphincter. The internal sphincter is present at the urinary bladder neck just above the prostate gland. The external sphincter is present in the urethra membranous part.
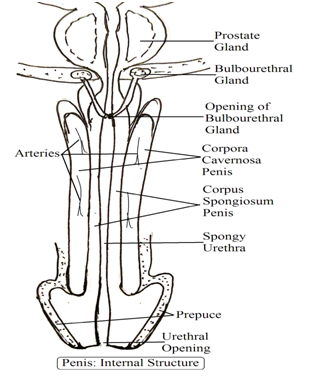
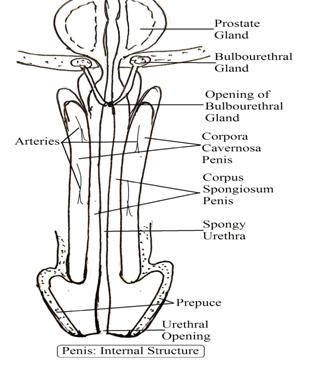
Penis: The penis is a long structure expanded at the tip and acts as a copulatory organ. The expanded tip of the penis is called glans. The glans of the penis have a slit opening known as urinogenital aperture. The glans of the penis are covered with a skin flap called foreskin or prepuce. The foreskin of the penis secretes sebaceous secretion known as smegma.
An erect penis is like a shaft. It had three columns of erectile tissue. Penis erectile tissues are two dorsal corpora cavernosa and one ventral corpus spongiosum. Corpus spongiosum enlarges at the penis end to form the glans (head) of the penis. It remains filled with blood during erection and also keeps the penile urethra open.
Wave-like contraction of penis muscle develops forceful discharge of semen. This is called ejaculation.
A pleasant sensation at the climax of coitus is called orgasm. It lasts for a few seconds.
Accessory Glands for the Male Reproductive System
There are three accessory glands associated with the male reproductive system. These are Seminal Vesicles, Prostate Glands, and Bulbourethral Gland(Cowper’s gland).
Seminal Vesicles: Seminal vesicles are a pair of musculo-glandular glands present at the base of the urinary bladder in the male pelvis.. Seminal vesicles produce Seminal mucoid alkaline fluid containing fructose, protein, phosphorus, and prostaglandin, seminal vesicle fluid constitutes about 60% of semen volume Alkaline fluid neutralizes male urethra acidity and female vaginal acidity. Acidic media inactivate and kill sperm. Fructose is sugar that acts as a source of energy for sperm.
Prostate Glands: It is a single-layered spongy grey-brown shape gland that secretes an alkaline milky fluid that constitutes 25% of semen volume. It nourishes and protects semen.
Bulbourethral Gland (Cowper’s gland): They secrete alkaline fluid. Its secretion is rich in mucus that lubricates the urinogenital tract and neutralizes urinary acidity.
Semen: Semen is a fluid containing sperms produced by the testes and various secretions secreted by seminal vesicles, prostate gland, and bulbourethral glands.
It is a milky viscous fluid, with a slightly alkaline pH of 7.3 to 7.5. It contains fructose, clotting factors, protein, phosphorus, and prostaglandins. It comes out from the penis during ejaculation.
The normal volume of semen ejaculated is 3 to 4 ml which contains 200 to 300 million sperms. In normal conditions, 60% of sperm must be vigorously motile.
The function of the Male Reproductive System
Spermatogenesis: The formation of sperm is called spermatogenesis.
Secretion of male sex hormone. (Formation of testosterone and androgens): Testes secrete testosterone that maintains secondary sex characteristics in males.
Storage of sperm: The male reproductive system stores and nourishes sperm.
Transfer of sperm: Male reproductive organ transfers semen into the female vagina during sexual copulation.
FEMALE REPRODUCTIVE SYSTEM
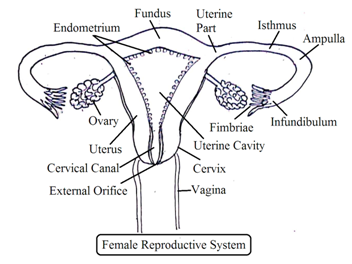
Anatomy of Female Reproductive System: The female reproductive system consists of internal reproductive organs and external reproductive structures called external genitalia (Vulva). The female reproductive system can be studied under three headings:
A. Internal Female Reproductive System,
B. External Female Reproductive system,
C. Female Reproductive organ Glands.
Internal Female Reproductive Organs
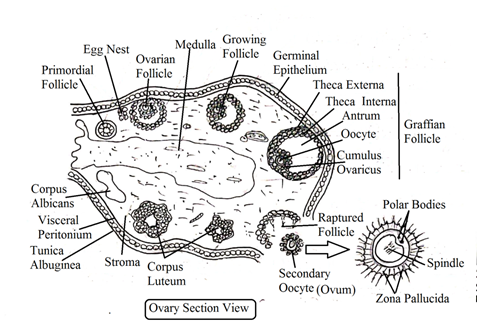
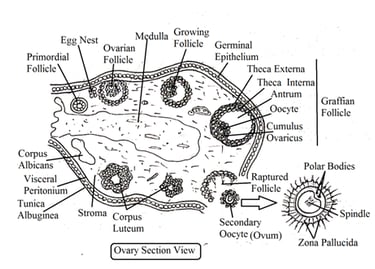
OVARIES: In the female reproductive system, the ovary is the primary sex organ. The female body has two almond-shaped grey-pink ovaries, one on each side of the uterus inside the pelvic cavity. Ovaries are attached to the uterus wall by ovarian ligaments. There are three parts of the ovaries. Germinal epithelium, Tunica albuginea, and ovarian stroma.
Germinal epithelium: Ovary outermost layers are made of squamous epithelium and cuboidal epithelium cells. These cells are commonly called germinal epithelium.
Tunica albuginea: It is made of connective tissue, present in between the germinal epithelium and cortex of the ovary
Ovarian stroma: Ovarian stroma consists of the outer cortex and inner medulla.
At the time of birth, both ovaries have 1 million to 2 million eggs (Oogonia). The body does not form any oogonia after birth. A large number of these Oogonia die (degenerate) between birth and puberty of females. Only 300000 oogonia remain in the female ovary at puberty. Only 500 Oogonia ovulate among 300000 Oogonia during the female reproductive lifetime. Only one Oogonium ovulates in 28 days inside adult female ovaries alternately. The remaining Oogonia die at menopause.
Oogonia form primary oocytes. These primary oocytes are called primary follicles. Primary follicles form secondary follicles. Secondary follicles are changed into tertiary follicles. Tertiary follicles have a cavity filled with fluid. The maturation of tertiary follicles forms mature follicles, known as Graafian follicles.
Functions of Ovaries: Ovaries perform mainly two functions. These are the secretion of the female sex hormone and the production of ova.
Female Accessory Organs:
The female reproductive system has three accessory ducts fallopian tubes (Oviduct), the Uterus, and vagina.
OVIDUCTS (Fallopian tubes): Each ovary is connected with the uterus by one fallopian tube. The length of the fallopian tube is about 10 to 12 cm. One end of the fallopian tube is in contact with the ovary and the other end remains in contact with the uterus. The fallopian tube has the following four parts: Infundibulum, Ampulla, Isthmus, and Uterine part.
i.Infundibulum: It is funnel-shaped at the end of the fallopian tube. This end has finger-shaped projections called fibre. It collects the ovum from the ovary after ovulation and provides passage for the ovum into the fallopian tube (oviduct).
ii. Ampulla: It is a curved, widest, and dilated part of the oviduct. Ovum fertilises in ampulla.
iii. Isthmus: It is a straight, short, thick-walled, narrow passage. Ampulla opens into it.
iv. Uterine part: This is the last part of the fallopian tube that opens into the uterus. It controls the movement of the ovum into the uterus.
The main function of the fallopian tube is to carry the ovum from the ovary, allow its fertilization inside the ampulla, and deliver the ovum into the uterus. Ovum movement in the fallopian tube is by peristaltic movement.
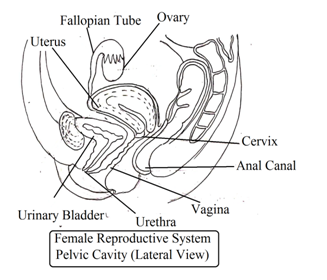
UTERUS): It is a hollow inverted pear-shaped structure between the rectum and urinary bladder inside the pelvic cavity. It consists of the following parts: fundus, body, and cervix.
The fallopian tube opens into the uterus. The fundus is the upper dome-shaped part of the uterus. The body is the middle part of the uterus. The body is also called the corpus. The cervix is the narrowest part of the uterus. The uterus is broader. The uterus is broader towards the fundus and narrows towards the cervix. The body opens into the cervix through internal OS. External OS of the uterus is circular.
The uterus wall has three layers. These are Perimetrium, Myometrium, and Endometrium. The perimetrium is the outer thin layer of the uterus. Myometrium is the thick muscular middle part of the uterus. The endometrium is an inner glandular layer of the uterus. Ovum after fertilization with sperm forms embryo. The embryo gets attached to the uterine wall and remains nourished and protected during the pregnancy period.
Vagina: It is about a 10 cm long elastic tube that acts as a female copulatory organ. It starts from the cervix and opens outside the body through the vaginal orifice. Some parts of the vagina surround cervix which is called the fornix.
In the vagina, the orifice is covered with a membrane called the hymen. Acidic media of the vagina inhibit the growth of other bacteria. But in the case of high acidity, it also kills sperm.
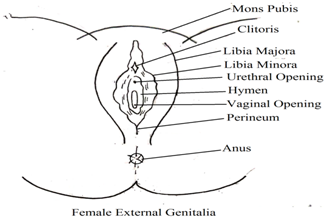
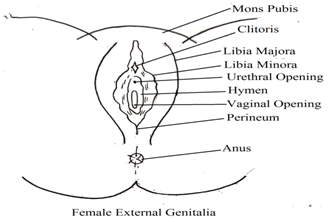
External Female Reproductive Organs
Vulva (External Genitalia): Vulva consists of Mons Pubis, Clitoris, Labia Majora, Labia Minora and Perineum.
Mons Pubis: Vulva anterior-most portion has a cushion of adipose tissues called Mons Pubis.
Clitoris: Clitoris is pea shaped erectile structure that resembles with glans penis of the male reproductive system. It is present just below mons pubis. It is a very sensitive part that erects with touch or any stimulation.
In female, urethral orifice and vaginal orifice are two separate openings for urine and vaginal discharge respectively.
Labia Majora: They are two large thick fleshy folds of skin that protect and enclose external female reproductive parts.
They are covered with pubic hair after puberty. They also contain sweat and oil-secreting glands (Sweat gland and sebaceous gland).
Labia Minora: They are two narrow fleshy smaller folds of skin present under Labia Majora. The area between both Labia Minora is called the vestibule. Vestibule is central depression in vulva.
Perineum: The area between the fourchette of labia minora and anus is called the perineum.
Female Reproductive organ Glands
The female reproductive system has two types of glands: Vestibular Glands and Mammary Glands
Vestibular Glands: There are two types of vestibular glands: greater vestibular gland and the lesser vestibular gland.
Greater Vestibular Glands: There are two red-yellow small glands. One vestibular gland is present on both sides of the vaginal orifice. They secrete a viscid, thick, alkaline fluid that acts as lubricant inside the vagina. They also neutralizes vaginal acidity. (Acidic media of the vagina kills sperm).
Lesser Vestibular Glands: They are small mucous glands. Large numbers of these glands are present on both sides of the urethral orifice.
Mammary Glands (Breast): Mammary glands are modified sweat glands to secrete milk. They are present inside round bulging on both sides of the thorax called breast. Each breast has pigmented dark color tip with multiple pores to release milk. This dark-colored tip is called a nipple. The skin near the surrounding area of the nipple has circular pigmentation. This area is called the areola. Areola has various sebaceous glands called the areolar gland.
Mammary glands develop during puberty. Hormone estrogen and progestron stimulate the development of glands at puberty. Each mammary gland consists of glandular lobes, connective tissues and adipose tissue.
a. Glandular lobes: Each breast has 15 to 20 glandular lobes made of various lobules. Each lobule has a grape-like cluster of alveoli. These alveoli secrete milk. Alveoli open into the mammary tubule. Mammary tubules open into mammary ducts. Near nipple, mammary ducts unite to form mammary ampulla. Mammary ampullae open into lactiferous ducts. Lactiferous ducts open outside the body through nipple pores. Mammary ampulla store secreted milk.
b. Connective tissues: Connective tissues in form of fibrous tissue are present among glandular lobes and give support to them.
c. Adipose tissues(Fatty tissue): Adipose tissues are present between glandular lobes. The numbers of adipose tissues decide the size and shape of the breast.
The function of Mammary Glands. After childbirth (Parturition) mammary glands of women secrete and release milk. This process is called lactation and women is called lactating women.
Milk Composition: Milk consists of fat droplets, milk protein (casein), milk sugar (lactose), vitamins, minerals, antibodies etc. Milk has a very minute amount of iron and vitamin C. Breast secretes colostrum just after childbirth. Colostrum is called first milk. But colostrum is not milk. Colostrum has antibody IgA that develops natural immunity in new born baby.
Ovulation
Ovulation is the process to release a secondary oocyte (ovum) from the ovary. Follicle-stimulating hormone (FSH) from the anterior pituitary gland stimulates the formation of mature ovarian follicles (Graafian follicle).
Graafian follicle secrete estrogen, a female sex hormone. Estrogen maintains female sex characteristics and makes the genital tract ready to receive the ovum. This release of the ovum from the ovary is called ovulation. (Ovary produces about 500 ova during entire female sexual reproductive periods). Ovum is released in mid of the menstruation cycle. After ovulation, many follicular cells collapse at the surface of the ovary. Collapsed follicles are filled with blood clot called corpus haemorrhagic. Follicle cells develop yellow carotene pigment (lutein)and called lutein cells. Lutein cells also release sufficient amount of progesterone. Collapsed follicular cells filled with blood clot fluid and lutein develops an enlarged yellow colour body called corpus luteum. The Corpus luteum also secretes hormone relaxin. Corpus luteum losses yellow colour. It stops the release of hormone slowly and corpus luteum degenerates slowly. This degenerated corpus luteum is called corpus Albicans (White body).
Ovulation: The release of secondary oocyte from the ovary is called ovulation. Ovulation occurs on the 14th day before the start of the next menstrual cycle. LH stimulates ovulation. Sperm combines with secondary oocyte inside the fallopian tube during fertilisation.
Menstrual Cycle
Female reproductive system undergoes physiological changes at an interval of 28 days (one lunar month) throughout reproductive life. These physiological changes cause discharge of endometrium lining with blood from the uterus of adult female at an interval of an average of 28 days. It is called the menstruation cycle. The menstruation cycle is regulated by hormones released by the pituitary gland. These hormones stimulate the ovaries to secrete ovarian hormones. Ovarian hormones affect the ovarian wall. Phases of the menstruation cycle:
Menstrual phase (Bleeding Phases or menses): First 5 days of the menstrual cycle in a human female is considered as a menstrual phase. It is associated with a decrease in the secretion of Luteinizing hormone (LH) from the anterior lobe of the pituitary gland. Reduction in LH level promotes degeneration of corpus luteum. This leads to a reduction in progesterone hormone level.
This causes the breakdown of the endometrium of the uterus and starts menstrual flow consists of blood, endometrium fragments and unfertilised ovum. In menstrual flow, blood does not clot due to the presence of fibrinolysin.
Proliferation Phase: It is also called the oestrogen phase. This phase lasts from the 6th day of the menstrual cycle to the 12th or 13th days of the menstrual cycle (28 days or a lunar month). The anterior lobe of the pituitary gland secretes FSH that stimulates ovarian follicles to secrete oestrogen. Oestrogen stimulates the endometrium of the uterine wall. Endometrium cells multiply rapidly become thick and rich in uterine glands as well as blood vessels.
Ovulatory Phase: On the 14th day of the menstrual cycle (about mid of menstrual cycle). LH and FSH are at the highest level. LH stimulates Grafian follicle to rapture and to release an ovum (secondary oocyte) that is ovulation.
Secretory Phase: It is also called the luteal phase. It lasts from the 15th day to the 28th day of the menstrual cycle.
During the secretory phase, two changes occur. One in the corpus luteum and another in the endometrium.
a. Corpus luteum: LH stimulates the release of ovum from Graafian follicle. After the release of the ovum, Grafian follicle becomes empty. The remaining follicular
cells form corpus luteum. Corpus luteum secretes hormone progesterone. Progesterone helps to maintain the endometrium.
b. Endometrium: Both LH and progesterone maintain the thickness of the endometrium. It helps in fertilized ovum implantation in the uterus.
The Corpus luteum degenerates if there is no fertilisation (union of sperm and ovum). It is the start of the next menstrual cycle.
Dr. Pramila Singh
